Ten Tips to Improve Iliosacral Screw Placement
Aprato A*, Devivo S and Masse A
DOI10.4172/2471-8416.100059
Aprato A*, Devivo S and Masse A
Department of Orthopedics, University of Turin, Turin, Italy
- *Corresponding Author:
- Alessandro Aprato
Department of Orthopedics, University of Turin, Turin, Italy
Tel: +393386880640
E-mail: ale_aprato@hotmail.com
Received date: August 03, 2016; Accepted date: February 09, 2017; Published date: August 16, 2018
Citation: Aprato A, Devivo S, Masse A (2018) Ten Tips to Improve Iliosacral Screw Placement. J Clin Exp Orthop Vol 4:59. doi: 10.4172/2471-8416.100059
Copyright: © 2018 Aprato A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Sacroiliac screw fixation has become the most common procedure for iliosacral joint fracture-dislocations and sacral fractures in the last decade. At present, the standard technique is the percutaneous iliosacral screw fixation under conventional C-arm fluoroscopy. This technique is considered to be a highly demanding operative technique with a high rate of screw malpositions, which may be associated with the risk of neurologic damage or inefficient stability. The surgical steps have been carefully described but, according to our experience, several tricks may be added to those descriptions. The purpose of this review is to summarize ten simple tips to help minimize failures and improve outcomes when positioning iliosacral screws.
Keywords
Sacroiliac joint; Cephalad projection; Screw placement; Iatrogenic injuries
Introduction
Although pelvic ring injuries are rare injuries, they present a challenge for the orthopadic surgeon. These fractures typically occur in young patients and are usually the result of high-energy traumas [1]. Based on these premises, the burden of these fractures is expected to be high [2,3], and the surgeon should try to minimize it.
Patients with unstable injuries are typically initially treated with a temporary fixation [4,5] until definitive surgery can be performed. Involvement of sacroiliac joint (SIJ) has been detected in about 30% of pelvic ring injuries [6] and definitive surgery often requires percutaneous iliosacral screw placement. This technique is considered to be a highly demanding operative technique with a high rate of screw malpositions [7,8], which may be associated with the risk of neurologic damage or inefficient stability. The surgical technique for percutaneous SI screw placement has been described in several papers [8] but, according to our experience, several tricks may be added to those descriptions. If these fractures are treated expeditiously, the most accurate reduction is achieved and fixation failures are minimized, patients will achieve better outcomes [9]. The purpose of this review is to summarize ten simple tips to help minimize failures and improve outcomes when positioning iliosacral screws.
TIP 1 Carefully evaluate the morphology of sacrum ala
Prior to start the procedure, careful preoperative plan is of critical importance to determine the success or failure of the procedure. Morphology of the sacral area should be evaluated to choose the best placement of the iliosacral screw and to avoid dangerous placement [10].
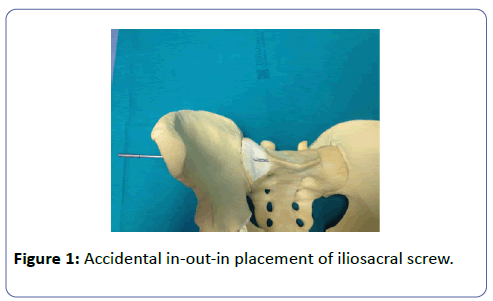
Complete and partial lumbarization of first sacral segment has been reported in about four percent of the population [10], this peculiar morphology may complicate a proper SIJ screw positioning: the screw may enter in the iliac ala, lie on the groove of the sacral ala then perforate the body of the first sacral vertebra (Figure 1). Avoiding this in-out-in placement is essential to minimize the risk of nerve injury: the l5 root lies close to the anterosuperior edge of the sacral ala and may be damaged by the drill or the screw itself.
This complication may be avoided with three simple tricks: proper detection of lumbarization of the saral ala may be done on the Xrays (anteroposterior pelvic view usually shows this deformity), in case of minimal deformity the sacral ala groove may be evaluated and measured on CT scan while, during surgery, a lower and more posterior entry point may be choose to avoid in-out-in placement.
TIP 2 Flex the leg to avoid problems with inlet view
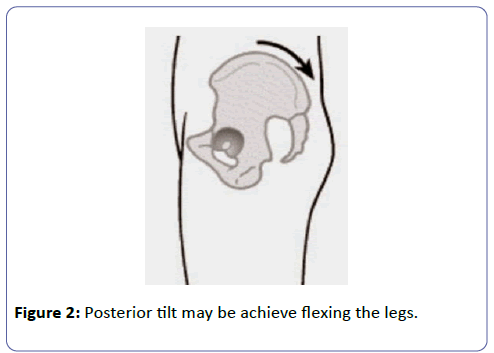
If SI screw is placed in supine position, a full radiolucent table is helpful but the technique may be performed also on standard surgical tables. Standard table may not allow the C-arm to rotate as much to achieve a proper outlet (cephalad projection) view because of the presence of table’s column. This view requires the beam to be tilted about 35 degrees [11] but in patients with hyperlordosis, the angle may be even higher, and the table column may prevent this angulation of the c-arm. Since a perfect view is essential to avoid screw malposition, two tricks may be useful to achieve this C-arm rotation angle: the patient may be moved toward the foot end of the table as much as possible and the hips may be flexed to reduce the pelvic tilt (Figure 2).
With the last trick a lower inclination angle is necessary to achieve a proper outlet view and perfect screw position may be performed bearing in mind to increase the opposite angle of the inlet view.
TIP 3 Design vertical and horizontal sacral planes on the skin
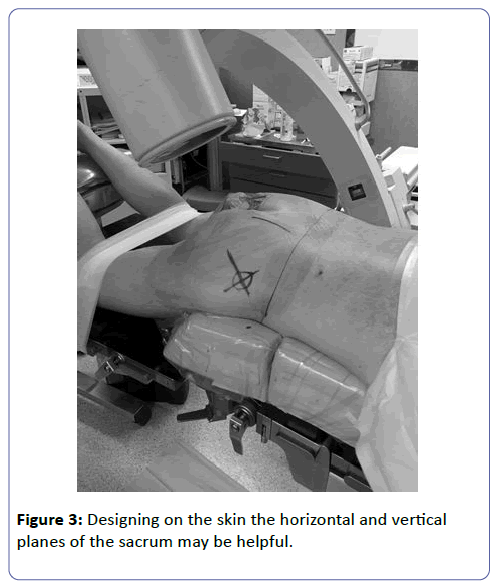
Before starting surgery a perfect lateral view of the sacrum should be performed to choose the best entry point but it allows the surgeon to design vertical and horizontal sacral planes on the skin. According to our experience, this little trick is very helpful to change the wire direction during its insertion, especially when the wire placement should be changed because it is satisfactory in only one between inlet and outlet view (Figure 3).
TIP 4 Carefully chose the entry point when dealing with crescent fractures
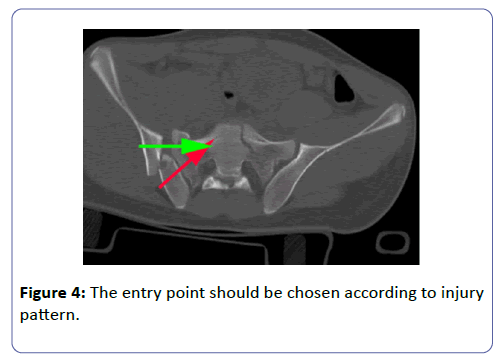
The so called “crescent fractures” involve a combination of ligamentous injury at inferior portion of SI joint, and vertical fracture of the posterior ilium which extends thru iliac crest [12,13]; in those cases posterior superior iliac spine remains attached to the sacrum therefore the risk of improper screw placement are higher. The choice of the entry point is essential in those cases and it should obviously be in the anterior part of the iliac ala (Figure 4).
Preoperative planning and intraoperative entry point choice are essential to fix the anterior portion of the ala and not the posterior spine to the sacrum. Starting point in the posterior portion of the ala will lead to a residual instability of the pelvic and to poor clinical outcomes.
TIP 5 Choose screw placement as orthogonal as possible to the dislocation or fracture
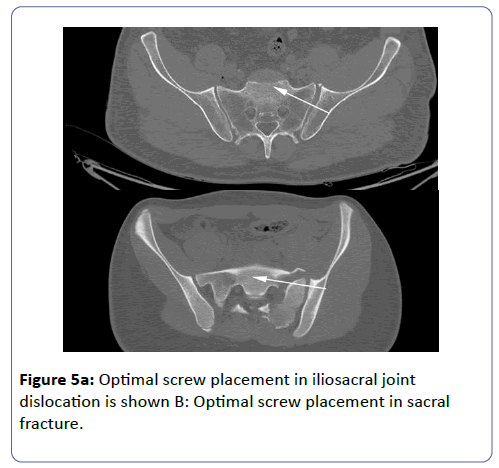
In case of SIJ dislocation, compression of the joint is though to be essential to achieve a complete fusion. To achieve this aim, screw should be placed as orthogonal as possible to the SIJ. Usually the entry point should be slightly posterior and the screw should direct anteriorly (Figure 5a). A perfect placement may help to compress the joint in order to improve the achieved reduction and to minimize the risk of future incomplete fusion.
On the other hand, a sacral ala fracture requires a screw placement as orthogonal as possible to the sacral sagittal line (Figure 5b). This may be achieved with a slightly anterior entry point and screw direction should be parallel to the horizontal plane of the surgical table. Again a perfect placement may help to give an optimal stability of the fracture’s fragments and will allow using a longer screw (see next tip).
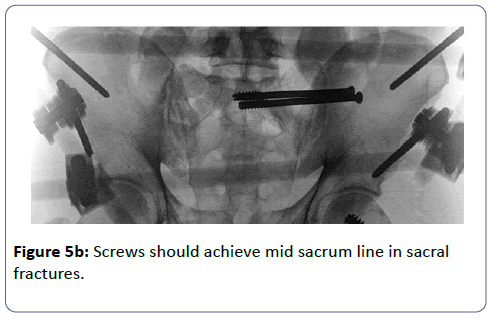
TIP 6 Screw should pass sacral midline for sacral fractures
As recommended in Tip 5, a screw placement as orthogonal as possible to the sacral fracture is the best solution for those cases. Furthermore to minimize secondary displacement and/or malunion screw’s length should exceed the half of the sacrum. This will increase stability of the fractures side involving the opposite hemi-sacrum into the resistance to displacement [14]. If the screw do not involve the opposite hemi-sacrum the fracture will be held by few millimeters of the screw tip in case of Denis [15] type 3 fractures, and this may lead to failure [8].
TIP 7 Avoid full length drilling
To increase the screw grip and the subsequent fracture stability we suggest to drill only the lateral iliac cortex, the medial one and the lateral sacral cortex. Avoiding to drill the full length of the wire is recommended to increase screw grip for two reasons: firstly the inside bone of the sacrum is cancellous and often weak; secondly screw tip is not fixed trough a cortical bone therefore its resistance to displacement is lower.
TIP 8 check the proper screw depth
Once the screw has been inserted, screw should be perfectly placed: either penetration into the iliac cortex either protusio of screw head should be avoided. Although easy in theory this step may be challenging because of the poor grip sensation due to surrounding soft tissues A combined inlet and obturator view may be helpful to chose the proper depth.
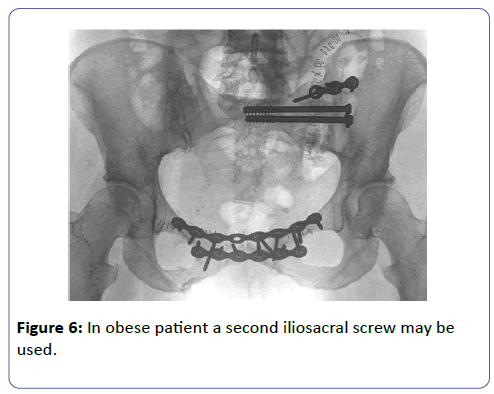
TIP 9 use a second screw in obese patients
According to our experience, obese patients present higher risk of secondary displacement therefore we suggest to use a second screw in patients with BMI higher than 30. A second screw may be placed in the second sacral vertebra [16] although this procedure presents the risks of nerve and vessels iatrogenic injuries (Figure 6).
TIP 10 avoid sitting after surgery for 40 days
Although most of the opinion leaders agree to avoid weight bearing for two o three months after iliosacral fixation [17], there is no consensus about limitation of sitting position. Our protocol recommend to avoid sitting angle over 40 degrees for 40 days after surgery. This recommendation is based on a published study [18] which demonstrated in simulation mode that sitting angle has a crucial influence in pelvis load and its intensity. Whether sitting at 90° the entire weight of trunk, upper limbs and head falls on the ischiatic tuberosities intensely stressing the structure, at 45° approximately 70% of the total load charges the pelvis and this percentage reduces to 26% at 15°. Those data show that pelvic fixation cannot bear a sitting angle above 45° without causing an out-of-range displacement of anterior and posterior complex. Although further study will be necessary to confirm or dispute those statement, we believe that sitting position should be avoided in the first weeks after surgery but we allow the patient to reach a position of 40 degrees for nutrition.
Conclusions
Sacroiliac screw fixation has become the most common procedure for iliosacral joint fracture-dislocations and sacral fractures in the last decade. At present, the standard technique is the percutaneous iliosacral screw fixation under conventional C-arm fluoroscopy and it may be used also for complex fractures or in abnormal sacral morphologies. Although screw malposition has been reported, with several technique tips the risk of suboptimal screw placement has been reduced therefore we suggest to use CT navigation only if the view with image intensifier is poor.
References
- Andrich S, Haastert B, Neuhaus E, Neidert K, Arend W, et al. (2015) Epidemiology of Pelvic Fractures in Germany: Considerably High Incidence Rates among Older People. PLoS One 10: e0139078.
- Aprato A, Joeris A, Tosto F, Kalampoki V, Rometsch E, et al. (2016) Are work return and leaves of absence predictable after an unstable pelvic ring injury? J Orthop Traumatol 17: 169-173.
- Aprato A, Joeris A, Tosto F, Kalampoki V, Stucchi A, et al. (2016) Direct and indirect costs of surgically treated pelvic fractures. Arch Orthop Trauma Surg 136: 325-330.
- Halawi MJ. Pelvic ring injuries: Emergency assessment and management. J Clin Orthop Trauma 6: 252-258.
- Nicodemo A, Decaroli D, Pallavicini J, Sivieri R, Aprato A, et al. (2008) A treatment protocol for abdomino-pelvic injuries. J Orthop Traumatol 9: 89-95.
- Rommens PM, Hessmann MH (2002) Staged reconstruction of pelvic ring disruption: differences in morbidity, mortality, radiologic results, and functional outcomes between B1, B2/B3, and C-type lesions. J Orthop Trauma 16: 92-98.
- Zwingmann J, Konrad G, Mehlhorn AT, Südkamp NP, Oberst M (2010) Percutaneous iliosacral screw insertion: malpositioning and revision rate of screws with regards to application technique (navigated vs. Conventional). J Trauma 69: 1501-1506.
- Zwingmann J, Hauschild O, Bode G, Südkamp NP, Schmal H (2013) Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg 133: 1257-1265.
- Routt ML Jr, Kregor PJ, Simonian PT, Mayo KA (1995) Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma 9: 207-214.
- Miller AN, Routt ML Jr (2012) Variations in sacral morphology and implications for iliosacral screw fixation. J Am Acad Orthop Surg 20: 8-16.
- Orchowski JR, Polly DW Jr, Kuklo TR, Klemme WR, Schroeder TM (2006) Use of fluoroscopy to evaluate iliac screw position. Am J Orthop (Belle Mead NJ) 35: 144-146.
- Shui X, Ying X, Mao C, Feng Y, Chen L, et al. (2015) Percutaneous Screw Fixation of Crescent Fracture-Dislocation of the Sacroiliac Joint. Orthopedics 38: e976-e982.
- Calafi LA, Routt ML Jr (2013) Posterior iliac crescent fracture-dislocation: what morphological variations are amenable to iliosacral screw fixation? Injury 44: 194-198.
- Kraemer W, Hearn T, Tile M, Powell J (1994) The effect of thread length and location on extraction strengths of iliosacral lag screws. Injury 25: 5-9.
- Denis F, Davis S, Comfort T (1988) Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res 227: 67-81.
- Khaled SA, Soliman O, Wahed MA (2015) Functional outcome of unstable pelvic ring injuries after iliosacral screw fixation: single versus two screw fixation. Eur J Trauma Emerg Surg 41: 387-392.
- Chen HW, Liu GD, Fei J, Yi XH, Pan J, et al. (2012) Treatment of unstable posterior pelvic ring fracture with percutaneous reconstruction plate and percutaneous sacroiliac screws: a comparative study. J Orthop Sci 17: 580-587.
- M Giachino, A Aprato, S Ali, A Bonanni, A Khattab, et al. (2014) Optimization of external fixation treatment in pelvic ring lesions by three-dimensional modelling and finite element analysis J Orthopaed Traumatol 15: S1-S17.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences