Abstract
Crossing screws versus tension band wiring for isolated non-comminuted olecranon fractures
Introduction: Several options continue to evolve for treating the common olecranon fractures. The reported high percentage of skin and implant related complications for these subcutaneous fractures raised the question about the need for a miniinvasive line of treatment that improves the results and minimizes the complications. Objectives: Prospective evaluation of the new line of treatment, crossing screws, versus the standard technique, Tension Band Wiring (TBW) in treatment of isolated non-comminuted olecranon fractures. Methods: A prospective study of 22 patients with Mayo type IIA olecranon fractures was conducted to evaluate the 2 techniques. They were divided into 2 groups: Group 1 included 11 patients treated by crossing screws and group 2 included 11 patients that were treated by TBW. Compression by the transcortical partially threaded screws applied in a crossing manner offers a stable fixation without soft tissue compromise that allows faster fracture healing and carry no danger for the skin. The patients were evaluated for operation time, quality of reduction, fracture healing, implant position, elbow range of motion, stability of fixation, and presence of complications. The functional evaluation was based on the Mayo Elbow Performance Score (MEPS). Results: All the fractures united in both groups in accepted position except one in group 2. No secondary procedure to achieve union was required only in that case. No fixation failure or implant migration problems were encountered in group 1, but, 2 cases in group 2. Faster radiographic union was encountered in group 1. One case in group 1 versus 2 in group 2 got superficial infection. No vascular or nerve complications were found. At a mean follow-up of 12.6 months (range 12-18 months), the elbow Range of Motion (ROM) and forearm rotation in group 1 were comparable to the intact side except 5 degrees extension deficit in 2 patients versus 2 patients with extension deficit 10 degrees and 2 patients with 5 degrees extension deficit. Using the MEPS, group 1 patients (100%) had a good to excellent results with a mean score of 94.3 (80-100), one patient had implant removal. In group 2, the mean score was 91.6 (75-95), with 6 cases had implant removal. Conclusion: Percutaneous or mini-open transcortical crossing screws for isolated non-comminuted olecranon fractures offered a cheap, simple and efficient mini-invasive stable fixation that allows early rehabilitation with excellent results and minimal complications. Their results were superior to the standard TBW. A multicenter comparative study is recommended before standardization of the technique
Author(s):
Mohamed Ali
Abstract | PDF
Share this

Google scholar citation report
Citations : 161
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
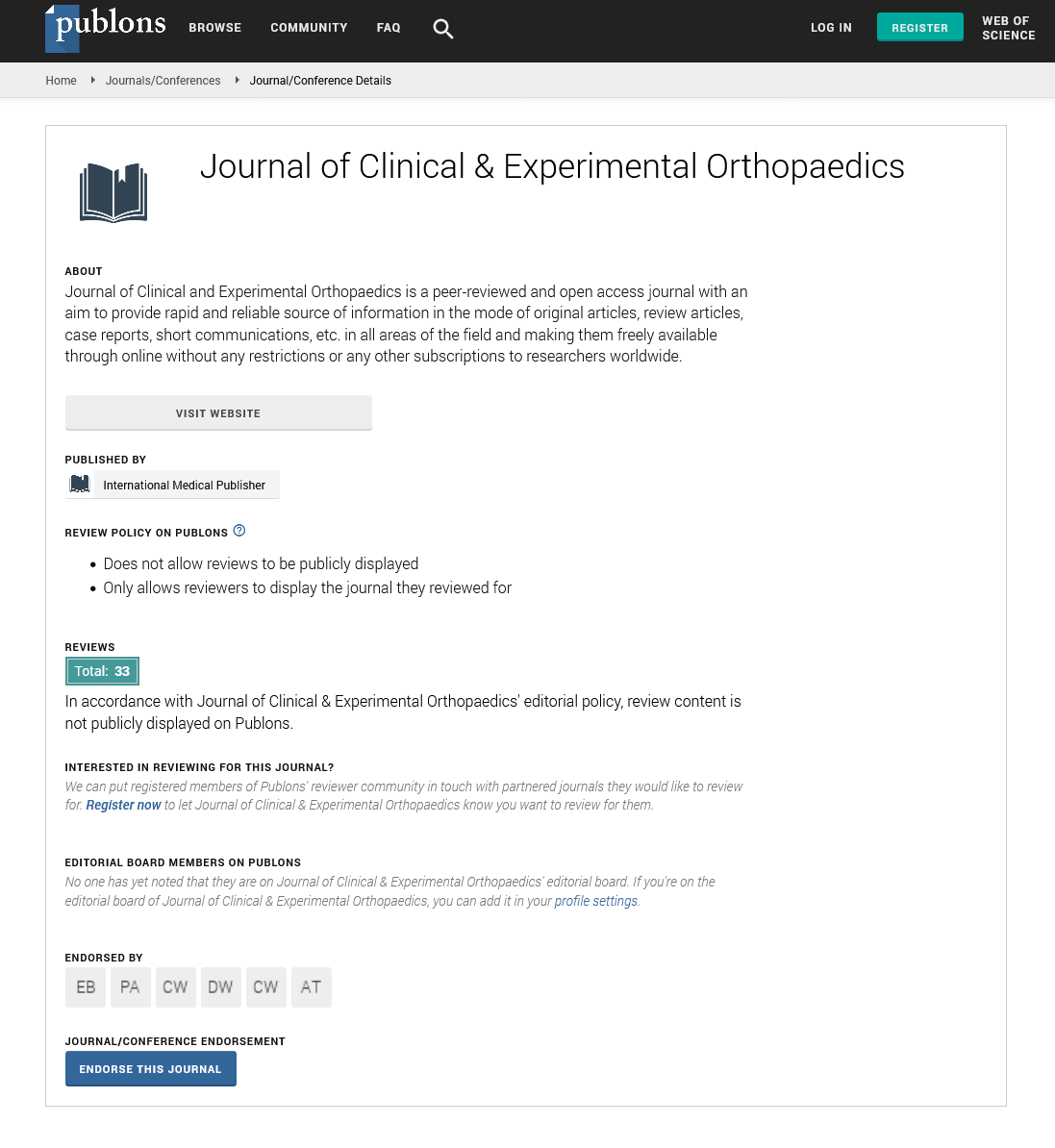
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences