Four Cases of Thoracic Ossification of the Ligamentum Flavum with Acute Progressive Myelopathy
Kurimoto Hisatsugu and Yokokura Satoshi
DOI10.4172/2471-8416.100043
Kurimoto Hisatsugu* and Yokokura Satoshi
Department of Orthopaedic Surgery, Teikyo University Hospital, Tokyo, Japan
- *Corresponding Author:
- Kurimoto Hisatsugu
Department of Orthopaedic Surgery
Teikyo University Hospital, Tokyo, Japan
Tel: +819091602544
Email: kurimoto0.82.7@gmail.com
Received date: October 26, 2017; Accepted date: November 03, 2017; Published date: November 09, 2017
Citation: Hisatsugu K, Satoshi Y (2017) Four Cases of Thoracic Ossification of the Ligamentum Flavum with Acute Progressive Myelopathy. J Clin Exp Orthop 3:43. doi:10.4172/2471-8416.100043
Copyright: © 2017 Hisatsugu K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Spinal cord paralysis symptoms due to ossification of the ligamentum flavum (OLF) often proceed slowly, and few reports have described acute progression of paralysis without any clear trauma that resulted in difficulty in walking. Here, we report 4 cases of thoracic OLF in which the patients had acute progression of myelopathy, and all had good recovery of paralysis after early decompressive surgery.
Conclusions: We report 4 cases of thoracic OLF with acute progression of myelopathy that required early surgery. Clinicians should consider the risk of acute progression of paralysis regardless of the type or level of OLF.
Keywords
Thoracic ossification; Ligamentum flavum; Paralysis; Surgery
Introduction
In our institute, from 2008 to 2013, we treated 4 patients who had acute progression of paralysis due to ossification of the ligamentum flavum (OLF) and required early decompressive surgery. All underwent laminectomies with the pedicles and facets preserved. Ossified sites were removed in 1 piece. All removed specimens were examined pathologically and were consistent with OLF.
Case Presentations
Case 1
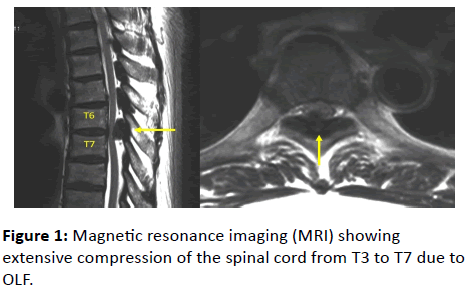
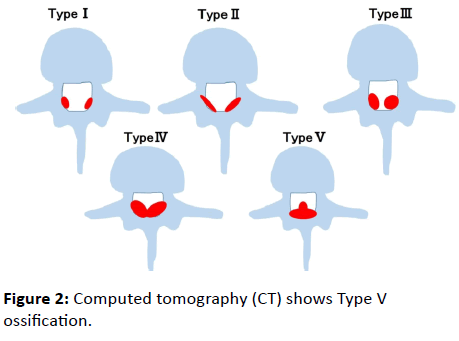
A 73-year-old man with no medical history presented with muscle weakness of his both legs and difficulty walking 4 weeks after the emergence of low back pain. His legs had gotten weaker over the 4 weeks and he became unable to walk. When he was admitted, muscle strength (manual muscle testing, MMT) was 3/3 in the iliopsoas (IP), 3/3 in the quadriceps femoris (Quad), 4/4 in the anterior tibialis (TA), and 4/4 in the extensor hallucis longus (EHL). Deep tendon reflexes were exaggerated bilaterally at the knees and the ankles. Babinski reflexes ware bilaterally positive. Paresthesia was noted below T7 level, and vesicorectal function was impaired. T2-weighed magnetic resonance imaging (MRI) showed extensive compression of the spinal cord from T3 to T7 due to OLF, which was especially prominent at T6/7 (Figure 1). Computed tomography (CT) showed Type V ossification (Figure 2).
The patient underwent surgery from a dorsal approach under general anesthesia. Laminectomy from T3 to T7 was performed; indentation of the spinal cord was confirmed. The patient was able to walk with a crutch at 4 weeks after surgery. His JOA score, excluding the upper limbs, improved to 8/11 at 1 year after surgery.
Case 2
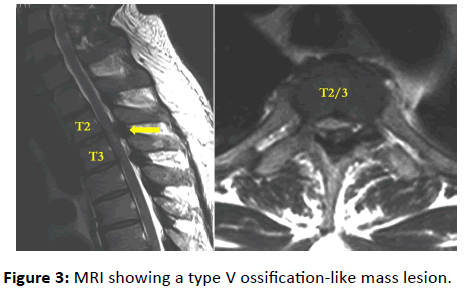
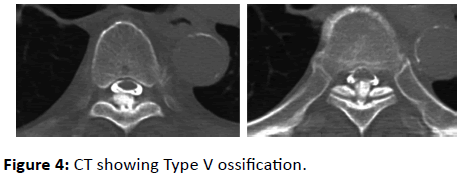
A 38-year-old man with no medical history was admitted because he became unable to walk over a period of 6 weeks after he began to feel numbness in both of his lower extremities. MMT results on admission were IP 2/2, Quad 3/3, TA 3/3, and EHL 2/2; and deep tendon reflexes were exaggerated. Babinski reflexes were bilaterally positive at the knees and ankles. Paresthesia below the T3 level was noted. His JOA score, excluding the upper limbs, was 4/11. MRI showed a type V ossification-like mass lesion, and T2-weighted imaging showed compression of the spinal cord from T2 to T4 due to OLF (Figure 3). CT showed Type V ossification (Figure 4). The patient underwent surgery via a dorsal approach under general anesthesia. Laminectomy from T2 to T4 was performed; ossification of the ligamentum flavum was identified, and indentation of the spinal cord was confirmed. The patient was discharged 4 weeks after the operation and was able to walk with a crutch. His JOA score, excluding the upper limbs, improved to 11/11 at 2 years after surgery.
Case 3
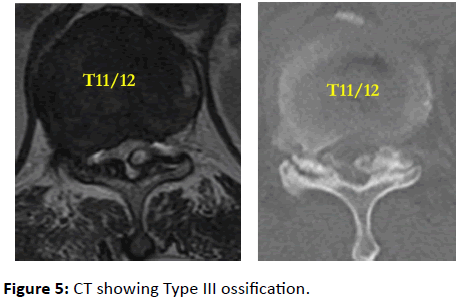
A 69-year-old man with a history of diabetes mellitus presented to another hospital with weakness of his left lower extremity and frequent urination and was referred to our institution for further detailed examination. MMT results on admission were as follows: IP 4/4, Quad 4/4, TA 5/5, and EHL 5/5. Deep tendon reflexes were exaggerated bilaterally at the knees. Babinski reflexes were bilaterally negative, and paresthesia below the T11 level was confirmed. His JOA score, excluding the upper limbs, was 4/11. T2-weighted MRI showed compression of the spinal cord due to OLF at T11/12. CT showed Type III ossification (Figure 5). Laminectomy at T11 and T12 was performed. The patient was discharged with a crutch 4 weeks after surgery. His JOA score, excluding the upper limbs, 6 months after surgery improved to 11/11.
Case 4
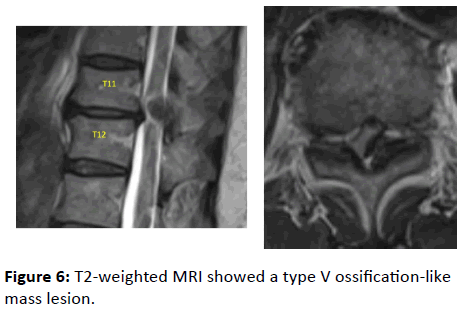
A 65-year-old woman was admitted to our institution due to difficulty walking, which rapidly emerged 3 weeks after she had developed weakness in her legs. MMT results on admission were as follows: IP 4/3, Quad 4/3+, TA 5/5, and EHL 5/4. Deep tendon reflexes were exaggerated bilaterally at the knees and ankles. Babinski reflexes were bilaterally positive, and vesicorectal function was not impaired. CT was not performed, but T2-weighted MRI showed a type V ossification-like mass lesion compressing the spinal cord at T11/12 (Figure 6). Her JOA score, excluding the upper limbs, was 6.5/11.
Laminectomy at T11 and T12 was performed, and she was discharged and able to walk 3 weeks after the operation. Her JOA score 1 year after surgery, excluding the upper limbs, improved to 11/11.
Discussion
In general, progressive transverse myeloplegia is a symptom of compressive myelopathy due to OLF [1]. In addition to pyramidal tract disorders, problems in the posterior funiculus have often been reported to occur due to compression of the posterior side of the spinal cord [2]. In this paper 2 of the 4 patients had difficulty walking even though their muscle strength was preserved with an MMT in the lower legs >4. Li et al. claim paralysis associate with OLF progresses slowly, and the average presentation occurs 9 months from the onset of symptoms [3]. It is comparatively rare that gait disturbance in patients with OLF proceeds so quickly that they need decompression surgery. Fong et al. reported a patient with acute weakness and numbness 1 week following left total knee arthroplasty [4] Li et al. reported a patient who presented with lower limb numbness and gait disturbance after minor trauma [5]. In our 4 patients, however, there were no episodes of trauma, and the exact mechanism of paraplesia is still unclear. Saito et al. and Igata et al. describe the following possible mechanism [2,5].
OLF gradually increases in size toward the spinal canal and compresses the spinal cord, making the spinal cord more fragile. They suggest that OLF leads to canal stenosis, which then results in obstruction of blood flow, and when the obstruction exceeds a certain threshold, acute onset of paralysis takes place. Moreover, it is possible that “above a certain threshold” could represent “minor trauma,” but “minor trauma” was not a common factor in our 4 cases. We speculate that minor irritation such as spinal concussion rather than spinal injury might have provoked myelopathy because myelopathy improved within a few weeks after early decompression, and there was no change in intensity seen on preoperative MRI.
Toledo et al. classified OLF into 5 types based on shape (Figure 2). In general, Type IV and Type V are more likely to cause paralysis [6]. However, in our 4 cases, there were no commonalities regarding the type of OLF or the level affected. We believe that OLF has the potential risk of acute progression of paralysis regardless of the type of OLF or the level affected.
Conclusion
We report 4 cases of thoracic OLF with acute progression of myelopathy that resulted in difficulty walking. Clinicians should consider the risk of acute progression to paralysis regardless of the type of OLF or the spinal level affected.
References
- Mori K, Kasahara T Mimura T, Nishizawa K, Murakami Y, Matsusue Y, et al. (2013) Prevalence, distribution, and morphology of thoracic ossification of yellow ligament. Spine 38: 1216-1222.
- Toledo J, Isseldyk FV, Re M, Garrote M (2013) Ossification of the ligamentum flavum as cause of thoracic cord compression: Case report of a Latin American man and review of the literature. Surg Neurol Int 4: 119.
- Li KK, Chung OM, Chang YP, So YC (2002) Myelopathy caused by ossification of ligamentum flavum. Spine 27 - Issue 12: 308-312.
- Fong SY, Wong HK (2004) Thoracic myelopathy secondary to ligamentum flavum ossification. Ann Acad Med Singapore 33: 340-346.
- Igata T (1977) Summary of thoracolumbar myelopathy, ossification of yellow ligament (Japanese). Clin Ortho Surg 12: 322-324.
- Saito K (1981) Two cases of ossification of the yellow ligament with acute progression of paralysis (Japanese). Kanto Journal Orthopedics Traumatology 12: 275-278.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences