The Characteristics of Two Sizes of the JuggerKnot Mini 1.0 mm: 2-0 and 3-0
Go Miake, Takamitsu Okada, Naohide Takeuchi, Takeshi Shimoto, Hidehiko Higaki and Yasuharu Nakashima
DOI10.4172/2471-8416.100024
Go Miake1, Takamitsu Okada1*, Naohide Takeuchi1, Takeshi Shimoto2, Hidehiko Higaki3 and Yasuharu Nakashima1
1Department of Orthopaedic Surgery, Graduate School of Medical Sciences, Kyushu University, 3-1-1 Maidashi, Higashi-ku, Fukuoka, Japan
2Department of Information and Systems Engineering, Faculty of Information Engineering, Fukuoka Institute of Technology, Fukuoka, Japan
3Department of Mechanical Engineering, Faculty of Engineering, Kyushu Sangyo University, 2-3-1 Matsugadai,Higashi-ku, Fukuoka, Japan
- Corresponding Author:
- Takamitsu Okada
Department of Orthopaedic Surgery, Kyushu University, Fukuoka, Japan
Tel: 81-92-642-5589
E-mail: tokada@ ortho.med.kyushu-u.ac.jp
Received Date: October 17, 2016; Accepted Date: November 07, 2016; Published Date: November 11, 2016
Citation: Miake G (2016) The Characteristics of Two Sizes of the JuggerKnot Mini 1.0 mm: 2-0 and 3-0. J Clin Exp Orthop 2:24. doi: 10.4172/2471-8416.100024
Copyright: © 2016 Miake G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: This study was to investigate the characteristics and the basic data of two sizes of the JuggerKnot Mini 1.0 mm.
Methods: Twenty-three 3-0 and thirty-four 2-0 anchors were inserted into synthetic bone, and we used twenty 3-0 and 2-0 anchors each which had been inserted correctly on the first attempt. After a preload of 10 N, cyclic testing was performed at 10-30 N for 200 cycles, after which destructive testing was performed. The parameters included the insertion form, the failure mode, the load to failure, and elongation at rupture.
Findings: 3-0 suture was more likely to be completely inserted at first insertion compared with a 2-0 suture. The mean strength of each anchor was 73.0 N and 118.7 N for 3-0 and 2-0, respectively. The average elongation at rupture of the 3-0 and 2-0 anchors was 2.63 mm and 3.66 mm, respectively.
Conclusions: These basic data and characteristics should be taken into account when using the JuggerKnot mini 1.0 mm in a clinical setting.
Keywords
JuggerKnot; Anchor; Cyclic test; Epoxy sheet
Introduction
Various commercially available suture anchors can be used for hand surgery. These include the Micro Quick Anchor (DePuy Synthes, Zuchwil, Switzerland), JuggerKnot Mini (Biomet, Warsaw, IN, USA), Micro Corkscrew (Arthrex, Naples, FL, USA). All of these types of anchors have been used in the reconstruction of hand ligaments or tendons [1-5].
The JuggerKnot has a radiolucent suture anchor body after implantation with various sizes, such as 1.0, 1.4, 1.5, and 2.9 mm. Several reports have described the strength of the JuggerKnot 1.4 mm [6,7], 1.5 mm [8], and 2.9 mm [8]. The JuggerKnot Mini 1.0 mm is a relatively new product, however, to our knowledge, no reports have described the basic data of this anchor since its release to market. The characteristic of these anchors should be clarified before they are employed in a clinical setting. In a market, we can use 2 different sizes of suture thread (3-0 and 2-0).
The purpose of the present study was to investigate the characteristics of the JuggerKnot Mini 1.0 mm with 3-0 and 2-0 suture thread and determine the basic anchor data for clinical use. Our hypothesis was that 2-0 suture was stronger than 3-0 suture because of its thread thickness.
Materials and Methods
Materials
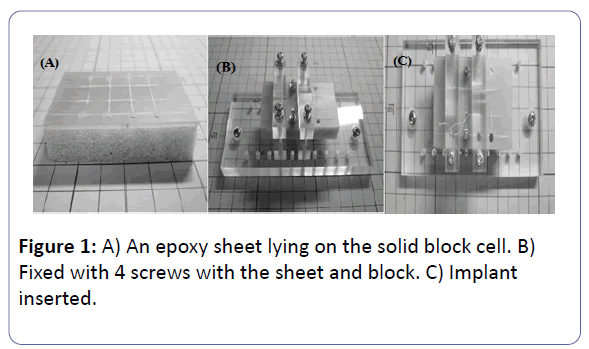
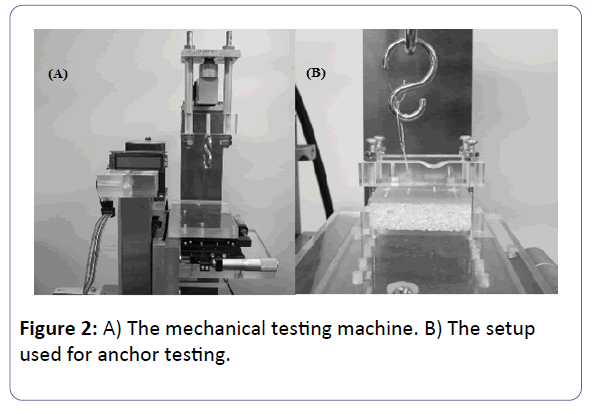
Biomet provided commercially available JuggerKnot Mini 1.0 mm (3-0, 2-0) anchors for use in the present study. Open solid cell foam [9] with a density of 20 pcf (Avice; Tokyo, Japan) and solid cortical epoxy sheet [10] with a density of 40 pcf (Sawbones; Pacific Research Laboratories, Vashon, WA, USA) was used to simulate bone. Solid blocks were chosen because their densities are uniform and because they offer higher specimen consistency than osteoporotic cadaveric or animal bone. We put a 60 × 35 mm epoxy sheet on a 60 × 35 mm piece of solid cell foam and fixed them with four screws (Figure 1). The anchors were inserted vertically and at least 10 mm apart to avoid cracking the epoxy sheet. The blocks holding the anchors were placed on an Instron mechanical materials testing machine (Model 5867, Instron Corp., Canton, MA, USA) (Figure 2A). A surgical knot was tied 3 cm above the cortical layer and fixed to the materials testing machine around an S-shaped hook (Figure 2B). Cyclic loading and pullout was performed vertically.
Test protocol
A preload of 10 Newtons (N) was applied. After the preload, cyclic testing was performed at 10-30 N at 0.5 Hz for 200 cycles [8]. A force of 30 N was applied because the maximum pullout strength of the 3-0 JuggerKnot should be approximately 70 N (the maximum strength applied during cyclic testing should be no more than half of the maximum pullout strength) [11]. Cyclic testing was performed by oscillating the panel, and the force was measured by a load cell (LC4102-K015, capacity: 150 N; A&D Orientec, Tokyo, Japan) attached to the upper S-shaped hook, which was connected to a computer via a strain amplifier (DPM-911B; Kyowa Electronic Instruments, Tokyo, Japan). The loading force was regulated by a computer-controlled AC servo motor (SGMPH-01BAA41; Yasukawa Electric Corporation, Fukuoka, Japan). Destructive testing was performed for the anchors which survived the cyclic testing at a displacement rate of 0.1 mm per second. The loading (N) data were recorded for every 0.02 mm of displacement. The force, which was determined using an Instron mechanical materials testing machine, was recorded on a computer. A custom-made software program was used to control the desired forces, the cyclic speed and the number of cycles.
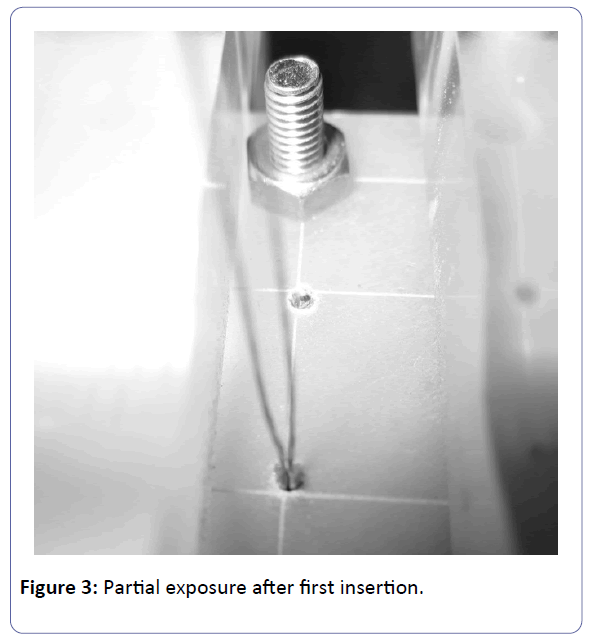
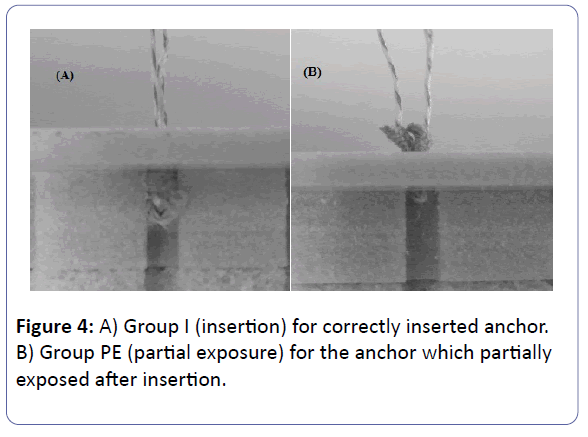
During our preliminary study, we found that some of the anchors that were inserted to the solid cell were partially exposed (Figure 3); these anchors could be manually pulled out with a low level of strength (less than 10 N). We therefore created two groups: the complete insertion group (Group I) for the anchors that were stable after the first insertion and the partial exposure group (Group PE) for the anchors which were partially exposed and appeared to have been inserted inadequately (Figure 4).
Our assessment criteria were distinguished in primary and secondary: i.e. a) quality of insertion, b) pullout strength. As for the quality of insertion, each test was performed until we reach 20 anchors in Group I. As for the pullout strength, we removed Group PE from the analysis because of the reason above. Parameters included the mode of failure (suture breakage or implant pullout), the load to failure (breaking force in N), and the elongation at rupture (mm) for each suture. The load to failure was considered to be the maximum load necessary to produce 3 mm displacement, suture breakage, or implant pullout.
Statistical analysis
At the onset of the study, a power analysis was performed to determine the number of anchors needed between groups. Using a preliminary data, with a α of .05 and a β of .80, we determined that 20 anchors were enough in each group. The values are presented as the means and standard deviation (SD). Pearson’s chi-squared test was performed to compare the number of groups, the number of failure modes, and the number of elongations >3 mm at rupture. Student’s t-test was performed to compare the load to failure and elongation at rupture (mm). P values of <0.05 were considered to indicate statistical significance.
Results
Quality of insertion
In total, we used twenty-three 3-0 suture and thirty-four 2-0 suture (Table 1). After insertion, the twenty-three 3-0 anchors were divided into Group I (n=21) and Group PE (n=2), and the thirty-four 2-0 anchors were divided into Group I (n=20) and Group PE (n=14). There was a significant difference in the number of each group (p=0.0074). Group PE was excluded for the reasons described above, and one 3-0 anchor of Group I was excluded with the following reason.
| Number: n* | ||
|---|---|---|
| Group I | Group PE | |
| Mar-00 | 21 | 2 |
| Feb-00 | 20 | 14 |
Table 1: Result of the number of groups in each anchor. *; A statistically significant difference was observed between the number of group of each suture by Pearson’s chi-squared test (p=0.0074). Group I: implantation group. Group PE: partial exposure group.
Pullout strength
3-0 sutures: After insertion, there was one anchor which did not survive the cyclic load test; it was pulled out 68 times during the cyclic load and subsequently removed from the study. In failure mode, failure occurred due to suture breakage (18/20 anchors) or implant pullout (2/20 anchors) (Table 2). The overall mean strength of the load to failure was 73.0 ± 12.5 N. The mean overall elongation at rupture was 2.63 ± 0.71 mm. eight anchors were displaced by more than 3 mm before reaching the maximum load.
| Failure mode: n | Load to failure*: N | Elongation at rupture†: mm | Elongation more than 3 mm‡: n | ||
|---|---|---|---|---|---|
| Suture breakage | Implant pullout | ||||
| Mar-00 | 18 | 2 | 73.0 (12.5) | 2.63 (0.71) | 8 |
| Feb-00 | 13 | 7 | 118.7 (16.9) | 3.66 (0.69) | 15 |
Table 2: Result of each anchor for Group I (insertion group). * †‡: A statistically significant difference was observed between the Load to failure, Elongation at rupture (mm) and the number of Elongation more than 3 mm of each suture by Student’s t-test and Pearson’s chi-squared test (p<0.0001, p<0.0001, p=0.0252, respectively).
2-0 sutures: As for the failure mode of 2-0, failure occurred due to suture breakage (13/20 anchors) and implant pullout (7/20 anchors). There were no significant differences in the number of failure modes for each anchor (p=0.0583). The overall mean strength of the load to failure was 118.7 ± 16.9 N. The overall mean elongation at rupture was 3.66 ± 0.69 mm. Fifteen anchors exhibited more than 3 mm of displacement before reaching the maximum load. There was a significant difference between the load to failure, the elongation at rupture (mm), and the number of elongations >3 mm of each anchor (p<0.0001, p<0.0001, p=0.0252, respectively).
Discussion
This paper was not a study reporting failures using JuggerKnot. This study was to understand the characteristics of the JuggerKnot mini 1.0 mm for its clinical use. The clinical relevance of this paper was to understand the characteristics of the JuggerKnot mini 1.0 mm, and based on this basic data, surgeons can decide which anchor for use.
Regarding the number of 3-0 and 2-0 anchors that were completely and partially inserted, 40% (14/34 anchors) of the 2-0 anchors were classified to Group PE, while 8.7% (2/23 anchors) of 3-0 anchors were incomplete insertion (Table 1). The same size suture anchor body and drill whole were used for the 3-0 and 2-0 sutures; thus, the only difference between the two experiments was the thread thickness. When the anchors were inserted into the drill holes, the 2-0 suture thread would occupy more of the hole (10.2 %) than the 3-0 suture thread (5.0 %) calculated from the mean diameter of the thread, and this might be the reason why more of the anchors were completely inserted with the 3-0 suture thread than the 2-0 suture thread. The thread thickness seems to have a significant relationship with the insertion form. In its clinical use, we suggest that surgeons should use another new anchor when the anchor becomes incomplete insertion.
As for the load to failure, the 2-0 sutures were significantly stronger than the 3-0 sutures (2-0: 118.7 N, 3-0: 73.0 N). As described above, the anchor bodies use the same fiber material; therefore, this increased suture strength results in higher failure loads that reflect the higher suture breaking strength. The size of the suture seems to be strongly associated with the anchor performance as we expected. However, we cannot simply compare our results with other studies because of the different materials used.
In our study, the mean elongation at rupture for the 3-0 sutures was 2.63 mm, while that of the 2-0 sutures was 3.66 mm (Table 2). Several suture analyses over the past 15 years have used 3 mm of suture-knot elongation to define “clinical failure” [12-14]. Knots that were tied with tails or “ears” that were left shorter than 2 mm were found to be more likely to unravel and to not hold reliably [15,16]. According to our results, “clinical failure” was less likely to occur with the 3-0 suture thread.
The present study is associated with some limitations, including the fact that this was a biomechanical, in vitro investigation. We used an epoxy sheet to ensure that the environment of each study remained the same and was conducted vertically. The traction force in vivo is different from that in our study. Data from this study therefore cannot be applied directly to the clinical setting. The results from the present study might differ from those of other biomechanical studies due to differences in the materials and methods used. Second, test protocols with or without a cyclic loading test may result in different data [6,8].
In summary, we investigated the basic data of the JuggerKnot Mini 1.0 mm with 3-0 and 2-0 suture thread in a biomechanical study. A 3-0 suture was more likely to be completely inserted at first insertion. We found that the strength of each anchor was 73.0 and 118.7 N for 3-0 and 2-0 sutures, respectively. The characteristic of the 3-0 suture was less likely to be the “clinical failure”. These basic data and characteristics should be taken into account when using the JuggerKnot mini 1.0 mm in a clinical setting.
Acknowledgements
This study was supported by an in-kind donation of medical devices, JuggerKnot Soft Anchors, from Biomet (Warsaw, IN, USA).
References
- Jarrett CD, McGillivary GR, Hutton WC (2010) The 2.5 mm PushLock suture anchor system versus a traditional suture anchor for ulnar collateral ligament injuries of the thumb: a biomechanical study. J Hand Surg Eur 35: 139-143.
- Kato H, Minami A, Takahara M, Oshio I, Hirachi K, et al. (1999) Surgical repair of acute collateral ligament injuries in digits with the Mitek bone suture anchor. J Hand Surg Br 24: 70-75.
- Latendresse K, Dona E, Scougall PJ, Schreuder FB, Puchert E, et al. (2005) Cyclic testing of pullout sutures and micro-mitek suture anchors in flexor digitorum profundus tendon distal fixation. J Hand Surg Am 30: 471-478.
- Lee SK, Kubiak EN, Liporace FA, Parisi DM, Iesaka K, et al. (2005) Fixation of tendon grafts for collateral ligament reconstructions: a cadaveric biomechanical study. J Hand Surg Am 30: 1051-1055.
- Morris SF, Yang D, Milne AD, Smyth BA (1999) Reconstruction of the proximal interphalangeal joint collateral ligaments using the Mitek Micro Arc Anchor: an in vitro biomechanical assessment. Ann Plast Surg 42: 124-128.
- Barber FA, Herbert MA, Hapa O, Rapley JH, Barber CA, et al. (2011) Biomechanical analysis of pullout strengths of rotator cuff and glenoid anchors: 2011 update. Arthroscopy 27: 895-905.
- Galland A, Airaudi S, Gravier R, Le Cann S, Chabrand P, et al. (2013) Pullout strength of all suture anchors in the repair of rotator cuff tears: a biomechanical study. Int Orthop 37: 2017-2023.
- Barber FA, Herbert MA (2013) Cyclic loading biomechanical analysis of the pullout strengths of rotator cuff and glenoid anchors: 2013 update. Arthroscopy. 29: 832-844.
- Yakacki CM, Griffis J, Poukalova M, Gall K (2009) Bearing area: a new indication for suture anchor pullout strength? J Orthop Res 27: 1048-1054.
- Kunkel KA, Rusly RJ, Basinger RR, DesJardins JD, Gerard PD (2013) In vitro acute load to failure and eyelet abrasion testing of a novel veterinary screw-type mini-anchor design. Vet Surg 42: 217-222.
- Ma CB, MacGillivray JD, Clabeaux J, Lee S, Otis JC. (2004) Biomechanical evaluation of arthroscopic rotator cuff stitches. J Bone Joint Surg Am 86A: 1211-1216.
- Burkhart SS, Wirth MA, Simonich M, Salem D, Lanctot D, et al. (2000) Knot security in simple sliding knots and its relationship to rotator cuff repair: how secure must the knot be? Arthroscopy 16: 202-207.
- Lo IK, Burkhart SS, Chan KC, Athanasiou K (2004) Arthroscopic knots: determining the optimal balance of loop security and knot security. Arthroscopy 20: 489-502.
- Rousseau B, Diop A, Atlan F, Priam S, Aim F, et al. (2013) Influence of prolonged immersion on the resistance of arthroscopy knots in biological media. Orthop Traumatol Surg Res 99: 138-144.
- Taylor FW (1938) Surgical knots. Ann Surg 107: 458-468.
- Tera H, Aberg C (1976) Tensile strengths of twelve types of knot employed in surgery, using different suture materials. Acta Chir Scand 142: 1-7.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences