Abstract
- Resistant HCV Variant after Cure Treatment with Ledipasvir/Sofosbuvir in a Patient with Chronic Hepatitis C
Currently, available standard treatment for patients with chronic hepatitis C (CHC) is a combination of direct-acting antiviral agents (DAAs) . ÃÂe results of the therapy of CHC with these DAAs show high sustained virological response (SVR) rates 80 - 90% but 1 - 15% failure to get this objective. DAAs are given in combination either to increase their e ô Ã?ectiveness or to prevent of hepatitis C virus (HCV) resistance-associated variants (RAVs) [3]. ÃÂe failures of treatment are usually seen when it’s relapsing or less oÃ?en to on-treatment viral breakthrough. ÃÂe host-virus related factors, the properties of the drugs used, and the treatment strategies are important in success of treatment. HCV RAVs persist for a long time depending on their types: NS3-4A variants disappear aÃ?er DAA therapy is stopped, NS5A variants persist for more than 2 years . ÃÂe best way to prevent the development of resistant variants is to eliminate the virus by the ýrst treatment administering DAAs which have high genetic barriers to resistance. In that point, ledipasvir/sofosbuvir (LDV/SOF) is recommended for treatment-naive or treatment-experienced patients with genotype 1, 4, 5 and 6 with or without cirrhosis by the guidelines . ÃÂe treatment duration with LDV/SOF and the need for the combination treatment with ribavirin (RBV) change to treatment experience, genotype and subtype and presence of cirrhosis. In genotype 1b treatmentexperienced patients with cirrhosis; 12 weeks of LDV/SOF without RBV in EASL, 12 weeks of LDV/SOF with RBV or 24 weeks of LDV/SOF should be used when RBV is indicated for 12- week regime and the individual is RBV-ineligible . In Health Implementation Guideline of Turkey, it is recommended that 12 weeks Case Presentation Our patient was a 58-year-old man with HCV diagnosed four years ago. He had no comorbidities and his brother was also diagnosed HCV. ÃÂere were no risk factors. His ýbrosis stage by Ishak was F5 four years ago and he was treatment-experienced with pegylated interferonRBV. On initial evaluation, he was asymptomatic and examination was unremarkable. Laboratory testing revealed elevated transaminase levels and HCV genotype 1b with a viral load of 4.2+E6 IU/mL. ÃÂe patient was treated with 12-week course of SOF (400 mg daily)/LDV (90 mg daily) and RBV (1000 mg daily). In the ýrst month of the therapy there was rapid normalization transaminase levels and clearance of the virus however, no side e ô Ã?ects of therapy has found. ÃÂe compliance of the treatment was certainly perfect. ÃÂree months aÃ?er completing treatment, virological relapse was occurred with a HCV RNA 4.0 +E5 IU/mL and his transaminase levels was slightly elevated. ÃÂis is shown clearly in Figure 1. Plasma samples, taken at the time of relapse were sent to Kocaeli University PCR laboratory for HCV sequence analysis to ascertain whether RAVs were present to account of LDV/SOF failure. ÃÂe patient was categorized as CHC according to the European Association for the Study of the Liver Clinical Practice Guidelines [6]. Blood sample with K2EDTA was immediately separated by centrifugation, liquated, and kept at -80Ã?C until required. ÃÂe presence of anti-HCV was tested for the sample which was anti-HCV positive through ELISA testing, using a commercial kit (Cobas E 601 Analyzer Roche Diagnostic- Mannheim, Germany). Histology was assessed according to the histological activity index (HAI) (grade) and ýbrosis (stage) by modiýed Ishak’s scoring of the liver biopsy. HCV RNA isolation and TuDntLýFDtLon Magnetic particle-based HCV RNA extraction and HCV RNA quantiýcation was performed using commercial real-time PCR assay – Abbott M2000 SP/Abbott RealTime HCV Ampli ýcation Kit (Abbott TagMan 2000, Illinois-Des Plaines USA). HCV NS3, NS5A and NS5B sequencing Genotypic resistance testing was performed three times by viral population sequencing of the NS3 region (amino acid position between 985. – 1295.), NS5A (amino acid position between 1935. – 2237.) and NS5B region (amino acid position between 2644. – 3054.) using an in-house method. ÃÂe primer pairs of the target designed against HCV strain AF483269.1. ÃÂe RT-PCR and the cycle sequencing thermal protocols were applied according to the manufacturer’s instructions. All PCR products were puriýed using the Highly Pure PCR Product 3uriýcation Kit (Roche Diagnostics GmbH, Mannheim, Germany) and directly sequenced with ABI PRISM 310 Genetic Analyzer equipment using the ABI PRISM BigDye Terminator Cycle Sequencing Kit (Applied Biosystems, CA, USA). ÃÂe sequences obtained with an electropherogram which were assembled using Vector NTI v.5.1 (InforMax, Invitrogen, Life Science 6oÃ?ware Frederick, MD). of 57 mm/hour. She had normal serum electrolytes with a plasma creatinine of 29 μmol/L but was hypoalbuminaemic at 25 g/L. She had a normal ASO titre of 104 IU/ml and a normal anti-DNAase-B of ‹100 µ/ml. She had normal complements C3 and C4 (1.32 g/L and 0.17 g/L respectively) with negative ANA, normal IgG of 11.8 g/L, IgM 1.0 g/L although elevated IgA at 1.9 g/L (normal 0.3-1.3 g/L). She had normal renal ultrasound without evidence of renal calculi. She had evidence of h\perfiltration injury with an increased formal51- CrEDTA glomerular filtration rate of 165 ml/min/1.73m2 . Her renal biopsy demonstrated IgAN with a di ô useÃ? mesangial proliferative glomerulonephritis and two of 29 glomeruli showing superimposed small segmental scars indicating previous focal segmental activity (Figures 1A Journal of Clinical & Experimental Orthopedics ISSN 2471-8416 and 1B). Immunohistochemical staining revealed strong di ô Ã?use granular mesangial IgA deposition with weaker IgM deposition but no deposition of IgG, C1q or C3 (Figure 1C). Electron microscopic examination demonstrated numerous mesangial and paramesangial electron dense deposits with scattered capillary loop deposits present in occasional areas She was commenced on an ACEI together with fñsh-oil supplements and had a further episode of macroscopic haematuria at six months aÃ?er presentation lasting two days associated with a febrile viral upper respiratory tract infection. At follow-up of three years, her proteinuria has decreased from 2+ to 1+ although she continues to have 2+ or 3+ intermittent microscopic haematuria. She has a normal urine albumin to creatinine ratio so her ACEI and fish-oil supplements have been discontinued. Her serum albumin has increased from 25 g/L to 44 g/L with a repeat formal glomerular filtration rate of 160 ml/min/1.73m2 Resistance associated mutation was analyzed by ÃÂe Genafor/ Arevirgeno2pheno drug resistance tool (Center of Advanced European Studies and Research, Bonn, Germany, http://coreceptor.bioinf.mpiinf.mpg.de/). HCV D90208 and HQ850279 were used as reference strains for the HCV NS3 - NS5A, and NS5B regions, respectively. In addition, for protease inhibitors; asunaprevir, boceprevir, faldaprevir, grazoprevir, pariteprevir, simeprevir, telaprevir, for NS5A inhibitors; daclatasvir, elbasvir, ledipasvir, ombitasvir, velpatasvir, and for NS5B inhibitors; dasabuvir and sofosbuvir were analyzed in the HCV NS3, NS5A and NS5B sequencing, respectively. Discussion Our patient was one of the among rare occurrences of the cases in whom viral relapse occur aÃ?er achieving end-of-treatment response with LDV/SOF. In spite of the compliance of the treatment, infected with genotype 1b and addition of RBV, with no reinfection and no comorbidity; the patient had only three poor prognostic factors: cirrhosis, male gender and treatment was experienced. Molecular analysis demonstrated that Y93H as a cross - resistant mutation for NS5A region related resistance mutation was determined. In addition, S282G and C316S were determined as amino acid substitution for NS5B region (Figure 1). NS5A resistance associated mutation (Y93H) could be e ô Ã?ective in relapse in LDV/SOF therapy . However, in Turkey, this case with Y93H mutation was to be reported ÃÂe mutation on position Y93 was described in 2012 and has then been well known to reduce the virus sensitivity to all NS5A inhibitors . ÃÂe rate of detection of NS5A RAVs is around 0.3 - 3.5%. ÃÂere are two RAVs in genotype 1b isolates that stand out: RAV L31M, which confer low-to-medium level resistance to ledipasvir and daclatasvir in 2.1 - 6.3% of patients, and RAV Y93H, which is the most frequently detected in 3.8 - 14.1% of patients. ÃÂese variants, more frequent in European patients (15%) in comparison to the USA (9.3%), confer medium-to- high level resistance to all drugs that inhibit NS5A In a study carried out by Garnier et al. ýve patients who relapsed aÃ?er sofosbuvir + daclatasvir treatment had emergence of a RAV . ÃÂose mutations were only detected aÃ?er relapse and were associated with resistance for the respective genotype of each patient: Y93N or M28T + Q30K for genotype 1a and Y93H for genotype 3. European guidelines do not recommend screening of RAVs before initiating antiviral therapy except for cirrhotic patients with genotype 1a before receiving simeprevir + sofosbuvir in CHC. While the last version of American Association for the Study of the Liver (AASLD) recommends resistance testing for RAVs only in patients who failed a NS5A inhibitor and are in urgent need to be retreated. However, repeated sequencing analysis with di ô Ã?erent plasma samples might be useful for the revealing the HCV RAVs in the relapse aÃ?er the cure treatments with DAAs. On the other hand, sequencing the NS5A region aÃ?er a relapse is necessary to help determine the next treatment regime
Author(s):
Figen Sarigul
Abstract | PDF
Share this

Google scholar citation report
Citations : 161
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
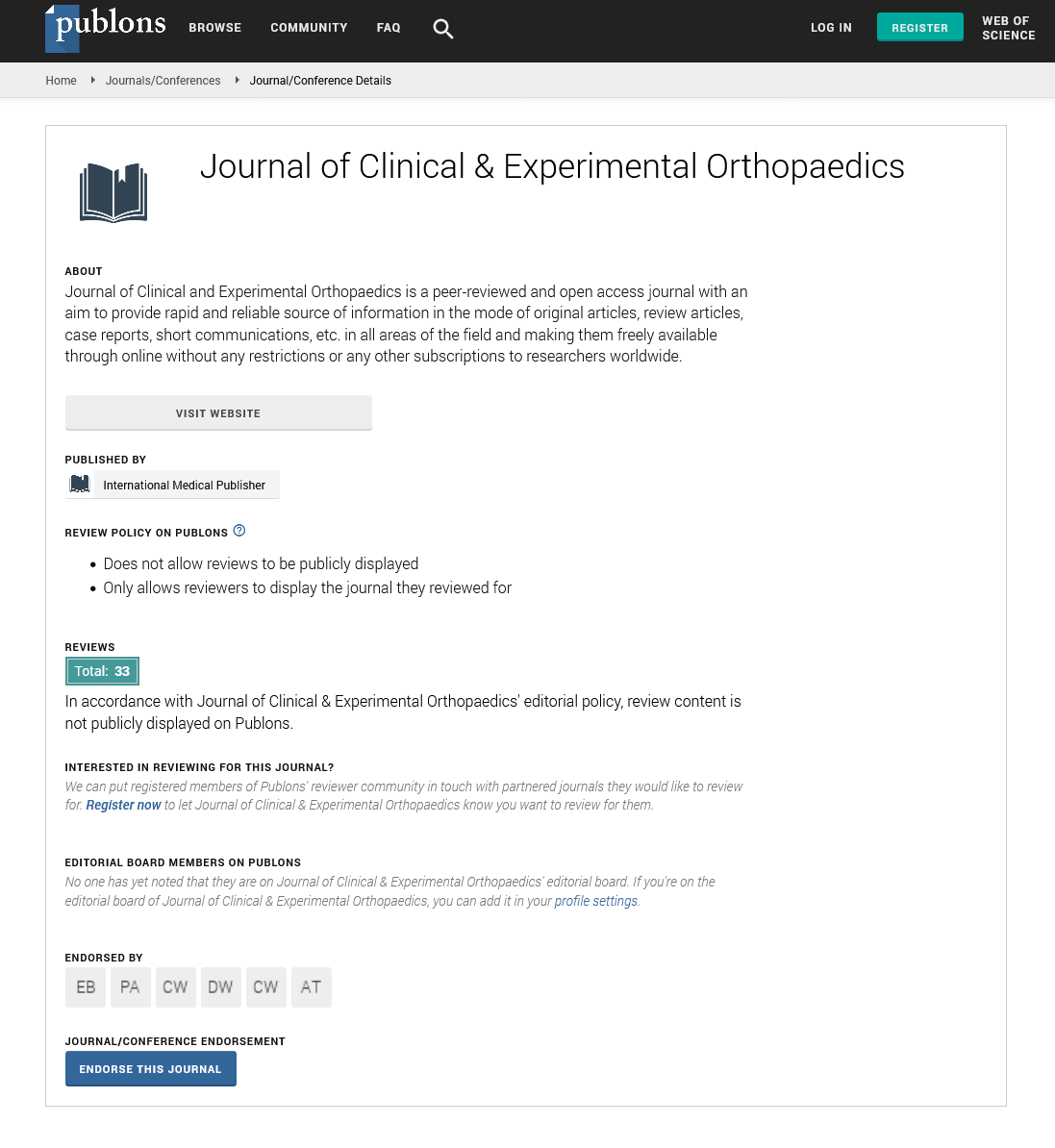
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences