Abstract
Bone Marrow Research in USA
Histology of CML The hypercellular marrow of CML shows panmyelosis and a virtual absence of adipocytes. There is granulocytic and/or megakaryocytic proliferation, eosinophilia and basophilia, occasionally with pseudoGaucher/sea-blue histiocytes and fibrosis. Past studies divided CML into two histological subtypes: a commoner granulocytic variant (~66%) showing unilinear granulopoietic hyperplasia, and a bilinear megakaryocytic type (~33%) additionally showing megakaryocytic hyperplasia, altered topology and pleomorphism with ineffective diminished erythropoiesis and grade 2-4 reticulin [1]. The clinical significance of this distinction (apart from the higher grade of fibrosis encountered in the megakaryocytic-type) remains controversial. Fibrosis in CML Manifest myelofibrosis is an adverse morphological factor associated with larger spleens, increased circulating blast percentages, lower hemoglobin levels and additional karyotypic abnormalities. Grading of collagen density, whether semiquantitative or by computerized morphometry, reveals that even slight increase in reticulin (compatible with doubled normal values) is associated with significantly worsened prognosis [2]. Thiele and Kvasnicka recommended that myelofibrosis should be included in any staging system in CML relating to survival Histological Changes in Therapy Imatinib mesylate therapy significantly decreases cellularity, neutrophil granulopoiesis, abnormal micromegakaryocytes, microvessel density and cell proliferation indices with regression of myelofibrosis. There is an increase in erythroid precursors and reactive lymphoid nodules with enhanced apoptosis. Myeloblasts, CD34+ cells and immature myelomonocytic cells also decrease in patients who go into complete or partial remission Imatinib-associated marrow aplasia has been described. Interferon-alpha induces apoptosis, resulting in reduced cellularity, expansion of normal erythropoiesis with increased iron-laden histiocytes and reticulum cells. Busalfan promotes myelofibrosis while hydroxyurea prevents it in a significant number of patients. In a study on 363 BMBs taken sequentially before and after allogeneic bone marrow transplantation, there was a significant correlation of marrow fibrosis, CD61+ cells and peripheral blood platelet counts with delayed haemopoietic reconstitution and leukemic relapse Ancillary Studies on the BMB Apart from assessing cellularity and fiber content, the BMB is also suitable for immunohistochemisty (angiogenesis, apoptosis, and proliferation indices) and morphometric studies as well as Fluorescent In-Situ Hybridization (FISH). Application of FISH to paraffin sections for demonstrating bcr/abl in intact cells, though not recommended for diagnosis, has been used as an adjunct to cytogenetic studies and to demonstrate the common stem cell origin of the CML clone. FISH for bcr/abl on BMBs was also found to be useful to monitor therapeutic efficacy of Imatinib Conclusion In conclusion, the BMB remains a valuable investigation in CML, both for the wealth of prognostic information conveyed as well as its usefulness in investigating scientific queries.
Author(s):
Kapil Verma
Abstract | PDF
Share this

Google scholar citation report
Citations : 161
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
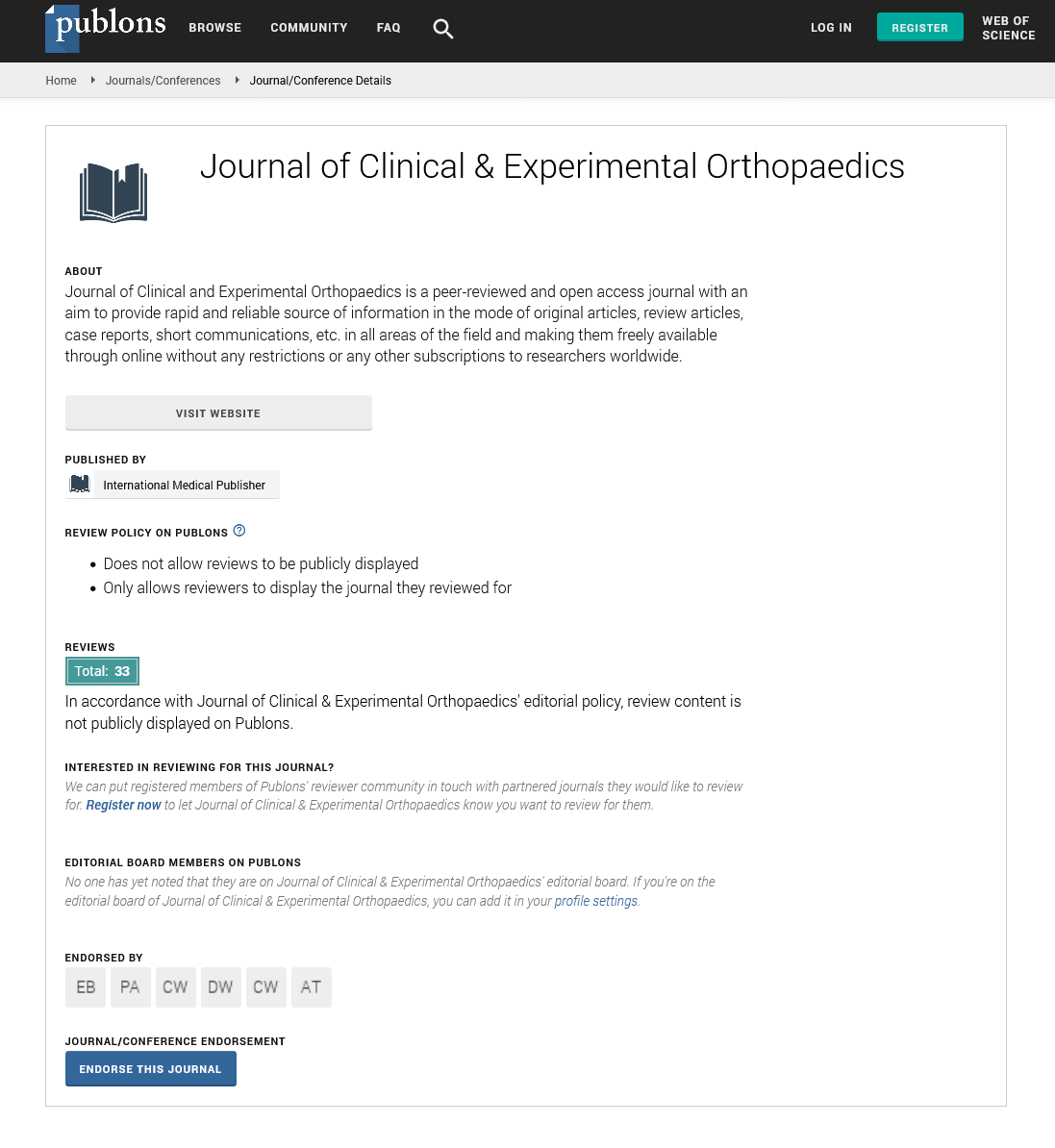
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences