Abstract
Combined Effect of Ultrasound and Laser Therapy (LLLT) for the Treatment of Pressure Ulcer in a Patient with Spinal Cord Injury
Pressure ulcer is a common complication aÃ?er spinal cord injury and is one of the leading cause of mortality. Prevalence of pressure ulcer is reported to be 4.9% in a study conducted at university hospital in India [1]. ÃÂere are many precipitating factors for ulcer formation. Intrinsic factors include sensory, autonomic, and motor impairment; obesity; malnourishment; and diabetes. Extrinsic factors include unrelieved pressure, friction, direct trauma, and inadequate skin hygiene [2]. Numerous physical therapy approaches to wound healing are described, including ultrasound (US), ultraviolet radiation. ÃÂere is sparse reference in recent literature to physical therapists' use of UV for wound healing. Existing literature concentrates on broad-spectrum UV light sources, predominantly A PA) and B (UVB) wavelength [3]. With electrical stimulation as a treatment modality it has been postulated that electrical current attracts fibroblasts and macrophages, improved wound microcirculation by directly stimulating local cutaneous nerves, and orient and a ô Ã?ect mesenchymal stem cell migration. But the application may pose certain challenges in terms increased chances of infection [4]. High voltage pulse current is also reported in the treatment of pressure ulcer but the benefit is mainly limited to pain relief rather than wound healing [5]. Physical therapists currently use US to treat wounds at a spatial average-temporal average (SATA) intensity of 0.1 to 0.5 w/cm2 [6]. Ultrasound dosages that clinically enhance wound healing have also been shown to produce cellular ultrastructural changes that are critical to normal healing [7]. ÃÂough there are conflicting evidences regarding the e ô Ã?ects of US, it still is a promising electrotherapy modality for tissue healing. Hogan, et al., claimed that pulsed ultrasound can promote circulation independently of a heating e ô Ã?ect He also found that US promotes angiogenesis. ÃÂis e ô Ã?ect may help in case of deep ulcers where tissue growth is important to cover the depth of an ulcer [7]. ÃÂe Low Level Laser ÃÂerapy is amplified in low light radiated power capable of promoting biochemical, bioelectric and bioenergetics ô e Ã?ects as a way of further treatment for the PU [8]. Adel J. Hussein, et al., reported the high phagocytic activity of macrophages during as early as 6 hours. LLLT can facilitate wound healing, which may be due to acute inflammation is resolved more rapidly and the proliferation phase of healing begins earlier, therefore, the LLLT decreased the inflammatory reaction of wound healing [9]. LLLT is also known for its e ô Ã?ects such as to accelerate the healing process, to increase tissue granulation, to decrease wound, to reduce inflammatory process and to reduce pain [10]. Considering the e ô Ã?ect of acceleration of healing process of LLLT for all types of pressure ulcers and angiogenesis e ô Ã?ect of Ultrasound which might prove to be beneficial for deep wounds, when a patient with deep pressure ulcer was referred to Physiotherapy, it was thought to study to combine e ô Ã?ect of LLLT and ultrasound in a patient of spinal cord injury with stage 2 pressure ulcer. In this article, healing of a pressure ulcer is described in detail measured with the help of PUSH scale. ÃÂe depth is measured separately with the help of inch tape. A 34 years old male patient with T4 fracture following road traùc accident came to Physiotherapy department aÃ?er 1½ months of injury. For this duration patient was admitted in another hospital and was bedridden. Patient also had fracture radius and ulna on right side which was treated conservatively. His chief complaints were inability to get up from lying position, diùculty in maintaining sitting position and inability to move both lower extremities. Score 12 in applying the Braden Scale (7), that is, high risk. As per the information gained from reliable informant, during the stay in another hospital, patient evacuated and urinated in diapers, keeping the wound with excessive moisture and possible contamination. As a result, a single class II pressure ulcer was developed on the sacral region with surface area of 24 cm2 . Evaluation of the ulcer was carried out by first author according to PUSH scale. It is a specific instrument for evaluating the PU healing process with three parameters: the wound area, the wound tissue type and exudates amount. ÃÂe sub scores for these parameters, when combined, generate a total score, which can range from zero to 17. Higher scores indicate worse PU and low scores indicates improvement in PU healing processes. On day 1 of the treatment, PU scored 12 on PUSH scale, with wound area of 24 cm2 . Wound area of PU was 4 × 6 cm in dimension measured in a greatest length (head to toe) and greatest width (side to side). Exudate amount was heavy in the first few weeks and wound tissue type was slough which is yellow or white tissue that adheres to the ulcer bed, recorded according to specifications given in PUSH scale. In addition depth was also measured with standard procedure using the cotton tip applicator. At the beginning the depth was 1.9 cm. Pressure ulcer was treated with ÃÂerapeutic Ultrasound and LASER. Ultrasound unit of India medico with a frequency of 3 MHz was used. Dosage was calculated according to the surface area and condition of the ulcer. To begin with the 0.8 W/cm2 intensity, pulsed mode was given. Water bag method was used for the treatment since PU was an Journal of Clinical & Experimental Orthopedics ISSN 2471-8416 open wound. A custom made water bag with the plastic glove filled with water was used. To avoid any infection a sterilized glove was used for each application and was placed directly over the PU. A gel was used as a medium for the smooth movement of ultrasound head. ÃÂe head was moved in all directions over the PU to avoid formation of standing waves. LASER ÃÂerapy was given by a Physiotherapist in Neurophysiotherapy unit by means of LASER Aluminum-GalliumIndium-Phosphorus (AlGaInP), with a wavelength of 660 nm (Po–30 W peak) brand Technomed with continuous light emission and pulsed once a day, six times a week for twelve consecutive weeks, with a total of 30 applications. At the edges of the PU, it was applied in with 4 J/cm2 for a fixed time and a distance between the points of 1 cm2 . In the center of the PU, application was given at a distance of 1 cm of tissue over a period of three to four minutes. ÃÂe laser used emits visible red light, which required the use of personal protective goggles for the eyes of the professionals in the application of therapy. ÃÂe patient did not need to use protective goggles, since the laser application was on his back. ÃÂe dosage was modified as the recovery took place. Routine nursing care of PU was continued without any interruption with cleaning and dressing of the wound on alternate days. Reassessment of pressure ulcer was done aÃ?er every two weeks (Figure 1). ÃÂe evaluation of the results aÃ?er the intervention was carried out reusing the PUSH scale for Wound Healing, measuring the depth of a PU. ÃÂis evaluation took place twice a week, over twelve weeks, always before the patient would receive physical therapy intervention and dressing interventions $Ã?er 1 week of intervention there was some reduction in the size of the lesion, which was, 4.2 cm of length, width of 6 cm and with an area of 25.2 cm2 . But still there was heavy exudate and tissue type was slough. ÃÂough there were no signs of infection or foul odour there was increased maceration and perilesional erythema. ÃÂere was no granulation tissue and epithelial tissue. ÃÂis clinical evaluation demanded stronger orientation to the nursing ô sta Ã? and family members about the need to control moisture in diapers, opting for the use of urine collector. Patient decubitus changes were intensified though with some diùculty to mobilize when sitting on the chair. $Ã?er 3 weeks, the size of the pressure ulcer reduced to 4 cm of length, width of 5.8 cm and with an area of 23.2 cm2 . Amount of Exudate was still in large quantity and there was no granulation tissue. ÃÂough the borders of ulcer were defined with some sign of healing, depth was still a challenge. ÃÂere was no foul odour. Routine nursing care was given along with frequent change of position. ÃÂis is a first study to report the combined e ô Ã?ect of LLLT and Ultrasound in the management of pressure ulcer in a patient with Spinal Cord Injury. ÃÂere was a significant decrease in the size of pressure ulcer from 24 cm2 to 0.1 cm2 . ÃÂere was also a significant decrease in the depth of a wound from 1.9 cm to 0.1 cm. LLLT accelerated tissue proliferation and increased local vascularization, with granulation tissue formation by promoting rapid healing of the lesion. Whereas, ultrasound clinically enhances wound healing by producing cellular ultrastructural changes that are critical to normal healing. ÃÂe time taken for the recovery is more as compared to the reported literature, probably because of the more depth of PU and the type of tissue in the current PU. Other studies have not mentioned the depth of a PU which is an important factor for healing to take place. Also, the case study reports the tissue type to be granulation tissue right from the 1st assessment whereas in the present study, the tissue type was slough for first 3 weeks. Hence, the healing was slower in the initial weeks i.e. upto 3rd week. As the granulation tissue started appearing from 4th week onwards, healing is seen to be faster. ÃÂerapeutic e ô Ã?ects of LLLT and Ultrasound, in combination must have resulted in complete recovery of PU. At the beginning it was necessary to replace slough with granulation tissue so that faster recovery can take place. Proliferative e ô Ã?ect of LLLT must have helped to reduce the inflammation and to accelerate the wound healing. New cell growth was necessary to fill up the depth of a PU which might have occurred due to the angiogenesis e ô Ã?ect of Ultrasound. ÃÂis was evident aÃ?er the granulation tissue that was formed aÃ?er 3 weeks. PUSH is the standard scale used for the assessment of wound and used widely but Nursing Outcome &lassification [11] is another tool used for the assessment of wounds which the authors came across during their literature review while writing the article. It is a better tool as compared to PUSH scale as it many other aspects of wound are covered in it, such as odour, type of drainage, surrounding skin, periwound oedema. However, NOC also does not include depth of a wound as one of the parameter. Hence a more comprehensive tool can be developed for the assessment of a wound which will include all the parameters. Further studies can use NOC classification for better assessment of a PU.
Author(s):
Suvarna Ganv
Abstract | PDF
Share this

Google scholar citation report
Citations : 161
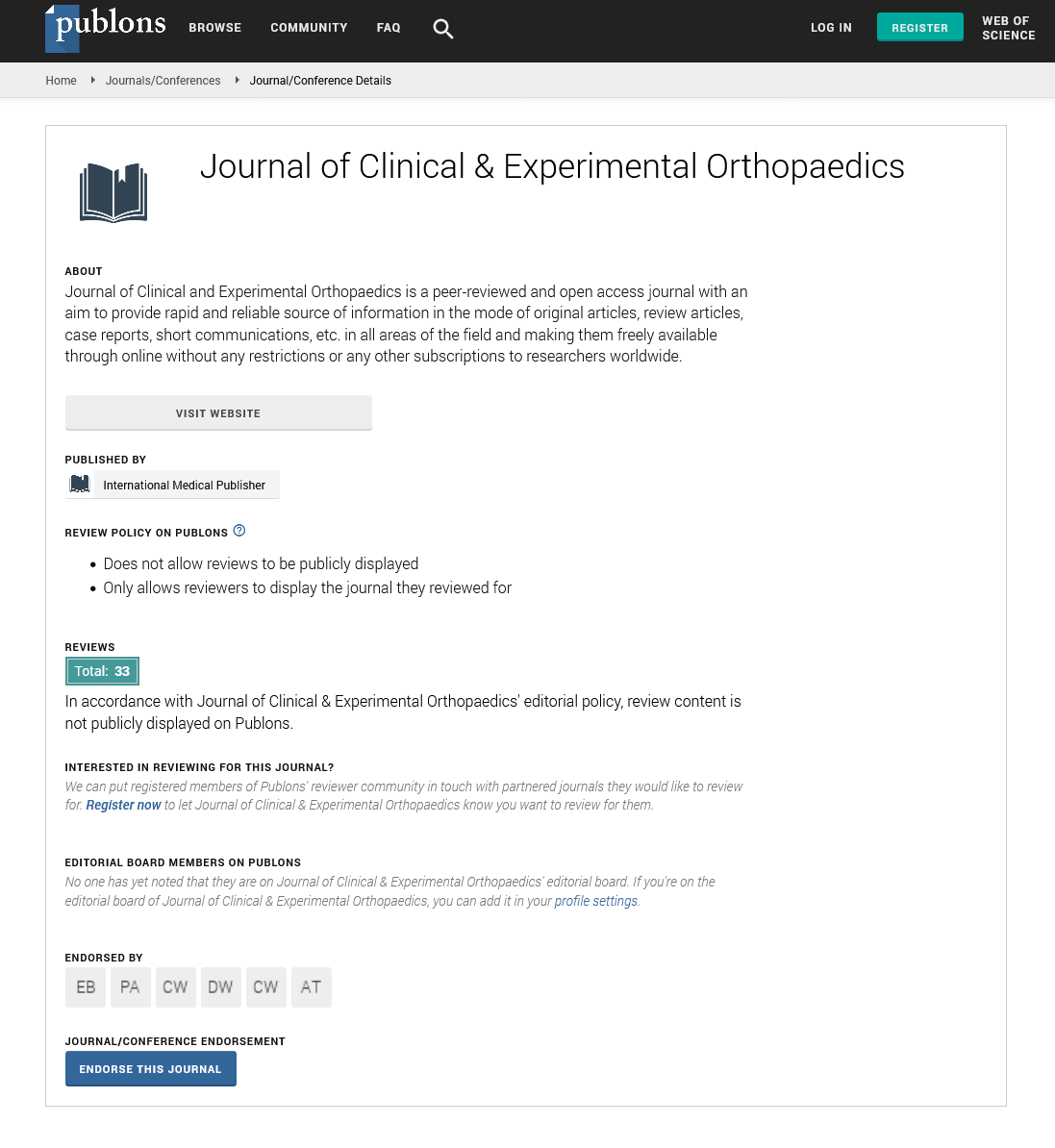
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences