Abstract
New Horizons in the Treatment of Cartilaginous Pathology beyond Conservative Secondary Prevention
Cartilage has traditionally been considered an inert tissue that develops in the early years and subsequently loses its capacity for repair and remodeling. Hence, all but the mildest injuries and degenerative conditions affecting the cartilage of joints have traditionally been treated conservatively with a view to reduce further harm and postpone the inevitable onset of symptoms rather than healing. Although these strategies remain the mainstay of treatment, cell and growth factor based therapies have recently shown great promise in the treatment of cartilaginous injuries and degenerative joints. In this month’s issue of the Journal of Physiotherapy and Physical Rehabilitation, we would like to report on new possibilities in adjunct therapies that do not yet have wide currency and would benefit from further research and circulation. Intraarticular injections of platelet-rich plasma (PRP) have been demonstrated to provide relief and improve function in osteoarthritis of the knee [1,2]. Activation of the PRP leads to the release of growth factors from the α-granules in the platelet cytoplasm. These growth factors have been associated with the initiation of a healing cascade that leads to cellular chemotaxis, angiogenesis, synthesis of collagen matrix, and cell proliferation [3]. As PRP has gained traction, some researchers have already considered combining this with other additives, such as growth hormone, which has shown to be promising [4]. Most studies have focused on injecting knee joints and hips, however, a new horizon is the extension of this treatment modality to other joints, such as the articulations of the spinal column. Pettine et al. [5] found that injection of autologous bone marrow aspirate was effective as an alternative to surgical vertebral fusion in reducing discogenic back pain. A paucity of published, randomized, controlled trials precludes us from evaluating the efficacy of these treatment modalities. Furthermore, it is uncertain if and how rehabilitation programs ought to be modified in patients receiving these adjunct treatments by physical therapists and rehabilitation specialists. As evidence mounts in favour of cell and growth factor based therapies, further research should be directed to studying whether combination with physical therapy modalities can further improve outcomes. This strategy, of course, presumes a simple mechanical model for the development of lower back pain. Recent studies have suggested alternate causes of intervertebral disc herniation and degeneration, such as infectious and inflammatory processes. Albert et al. [6] found improvement in lower back pain after long-term antimicrobial therapy, providing strong support for a role of Propionebacterium acnes in lumbar spondylosis. Others have also found a high prevalence of microorganisms in extruded disc material [7,8]. Lest anyone doubt the plausibility of this hypothesis, Chen et al. [9] have been able to demonstrate P. acnes as a causative factor in an animal model. A new-found association between aquaporin-1 expression and lumbar disk herniation has also been discovered [10]. This offers researchers a new avenue for investigation regarding the aetiology of intervertebral disk herniation symptoms. These advances in the field of musculoskeletal pathology have the potential to revolutionize the approach to cartilaginous and degenerative conditions in terms of prophylaxis and targeted treatment modalities. Given that more than half of herniated discs will spontaneously resorb [11], the great call for conservative treatments should continue to resound. However, those herniations that remain can cause lasting neurological sequalae if left untreated, which demands rigorous identification of patients that are unlikely to experience improvement without invasive surgical-intervation
Author(s):
Wegrecki KJ
Abstract | PDF
Share this

Google scholar citation report
Citations : 161
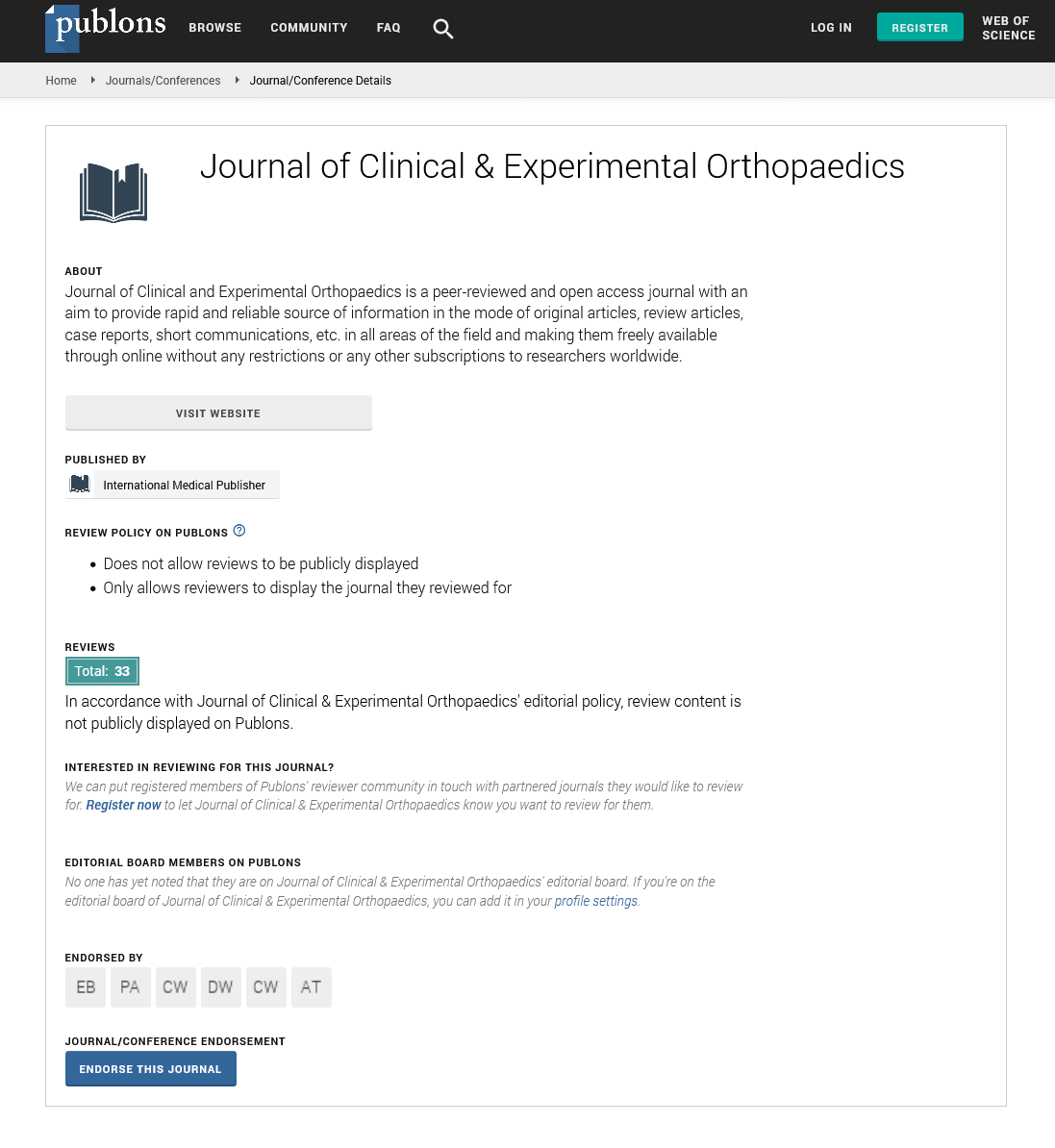
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences