Abstract
The Youngest Paediatric Presentation of IgA Nephropathy
IgA nephropathy is the most common form of glomerulonephritis identified in paediatric renal biopsies of children. Up to 40% of percutaneous renal biopsies are performed in children due to macroscopic haematuria and/or proteinuria. ÃÂe prevalance of IgAN may be underestimated as the disease may present with adultonset end stage renal failure (ESRF) without previous childhood history. Eighteen percent of patients show progression of renal disease within ten years aÃ?er the first renal biopsy and long-term outcome studies predict that 10-20% of adult patients will develop ESRF within ten years [1]. Detecting IgAN early in its natural history may ô o Ã?er the possibility of treatment to prevent progression of renal failure. ÃÂere is controversial evidence regarding the eùcac\ of treatment in IgAN with some randomised controlled trials supporting the beneficial e ô Ã?ect of either prednisolone or fish-oil supplements in regards to decreasing proteinuria and slowing the progression of renal impairment [2]. ÃÂe clinical decision to treat a patient who has IgAN with angiotensin converting enzyme inhibitors (ACEI) alone or to add immunosuppressive or other agents, largely depends on the presence of ongoing disease activity with proteinuria (which can also represent damage from previously active disease). A recent, multicentre placebo-controlled trial in children and young adults reported equal e ùcac\ of prednisolone, and fish-oil supplements in significantl\ reducing proteinuria compared to controls. Long-term follow-up of adults with IgAN appears to indicate the greatest benefit is achieved if treatment is started early in the course of the disease. We present the case of a young child presenting with IgAN who made a good response to therapy with follow-up of three years. A 26-month old girl presented with macroscopic haematuria, nephrotic syndrome without hypertension or renal dysfunction. She developed subsequent intermittent macroscopic haematuria for two months. She had no precipitating viral upper respiratory tract infection. She had mild peri-umbilical abdominal pain, not associated with loin pain. She had normal antenatal, postnatal history without past medical or family history of note with normal growth and development. On examination, she was well, with weight-height above the 50th centile, and normal blood pressure of 84/52 mmHg. She had only mild periorbital swelling. She had 3+ proteinuria and 3+ of haematuria on urinary dipstick testing with >500 red blood cells × 106 /L without white cells on urine microscopy. Her urine albumin:creatinine ratio was elevated at 253 mg/mmol without evidence of hypercalciuria. She had βhaemolytic streptococcus group G growing from her throat swab. She had a normal full blood count with haemoglobin of 14 g/dL and normal coagulation screen. She had an elevated ESR of 57 mm/hour. She had normal serum electrolytes with a plasma creatinine of 29 μmol/L but was hypoalbuminaemic at 25 g/L. She had a normal ASO titre of 104 IU/ml and a normal anti-DNAase-B of ‹100 µ/ml. She had normal complements C3 and C4 (1.32 g/L and 0.17 g/L respectively) with negative ANA, normal IgG of 11.8 g/L, IgM 1.0 g/L although elevated IgA at 1.9 g/L (normal 0.3-1.3 g/L). She had normal renal ultrasound without evidence of renal calculi. She had evidence of h\perfiltration injury with an increased formal51- CrEDTA glomerular filtration rate of 165 ml/min/1.73m2 . Her renal biopsy demonstrated IgAN with a di ô useÃ? mesangial proliferative glomerulonephritis and two of 29 glomeruli showing superimposed small segmental scars indicating previous focal segmental activity (Figures 1A and 1B). Immunohistochemical staining revealed strong di ô Ã?use granular mesangial IgA deposition with weaker IgM deposition but no deposition of IgG, C1q or C3 (Figure 1C). Electron microscopic examination demonstrated numerous mesangial and paramesangial electron dense deposits with scattered capillary loop deposits present in occasional areas IgAN is an immune-complex-mediated glomerulonephritis defined immunohistologically by the presence of glomerular IgA deposits accompanied by a variety of histopathological lesions. ÃÂe presence of glomerulosclerosis, crescents, interstitial fibrosis or tubular atrophy provide the most reliable histological indicators of poor outcome. ÃÂe percutaneous renal biopsy of our patient confirmed IgAN with a mesangial proliferative glomerulonephritis and mesangial deposition of IgA. A variety of histological parameters and classifications have been used to attempt to predict prognosis in patients with IgAN. ÃÂe International IgAN Network, working with members of the Renal Pathology Society, has established an international working group which is developing a consensus classification. Reports from di ô Ã?erent regions of the world indicate di ô Ã?erences in the pattern of disease class. Mesangial proliferation (subclass I and II) was predominant in a report from Macedonia where proliferative and cresentic forms were responsible for up to 30% of reported IgAN.As expected, the severity of renal histology, usually defined by focal sclerotic lesions or cresents, is associated with poor outcome for paediatric IgAN. Recent prospective studies showed that 40% of patients with as little as 10% cellular crescent will progress to ESRF [1,3,4]. IgAN and HenochSchönlein purpura nephritis (HSN) are histologically indistinct diagnoses and represent the most commonly occurring form of paediatric glomerulonephritis. ÃÂe clinical, genetic and immunologic features of these two conditions are so closely linked that one could consider HSN as the systemic form of IgAN. IgAN seems to be a renal-restricted form of HSN. In the majority of cases, Journal of Clinical & Experimental Orthopedics ISSN 2471-8416 IgAN is an isolated renal disease without systemic manifestations. Approximately 40-50% of patients present with recurrent macroscopic haematuria, which usually coincides with mucosal infections or exercise. Asymptomatic macroscopic haematuria with or without proteinuria is the presentation in 30-50% of most series. However, IgAN and minimal change disease have previously been reported as co-existing together in children. Our case also presented with nephrotic syndrome and recurrent macroscopic haematuria but her biopsy demonstrated IgAN with mesangial IgA deposits, confirmed with electron-dense deposits in the same distribution on electron microscopy [5-7]. Previous reports have suggested that the outcome of childhood IgAN is age related. ÃÂere was a peak in poor outcomes among patients diagnosed aÃ?er the age 16 years.
Author(s):
: Kibriya Fidan
Abstract | PDF
Share this

Google scholar citation report
Citations : 161
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
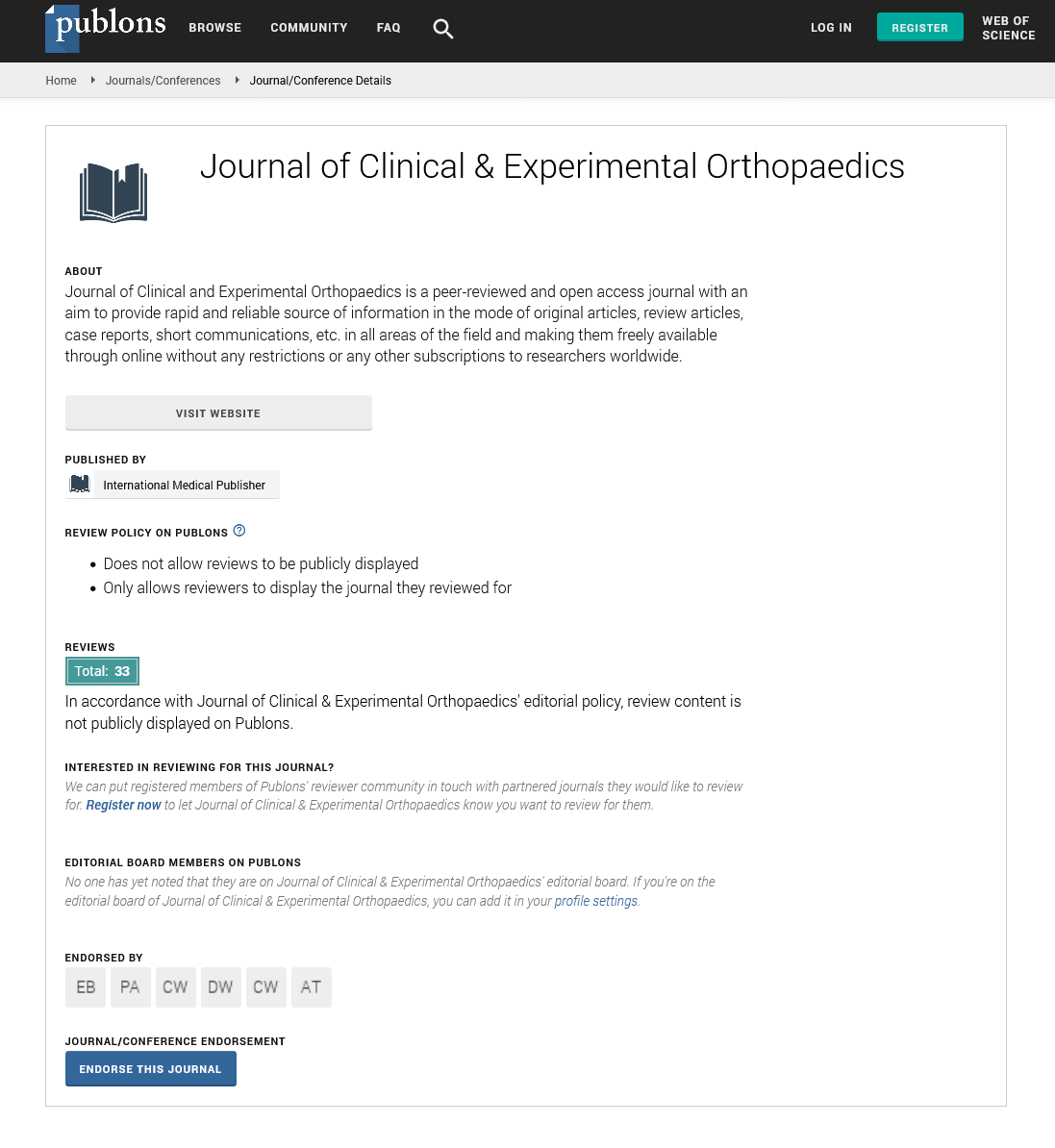
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences