Abstract
Treatment Response Monitoring in Patients with Multiple Myeloma: The Role of Positron Emission Tomography-Computed Tomography using Fluorine-18-Fluorodeoxyglucose
Multiple Myeloma (MM) is a common haematological condition primarily affecting older people, with a median age at diagnosis of about 65-70 years and a slight prevalence in male gender and in AfricanAmericans [1]. An abnormal plasma cell growth within the bone marrow accounts for this condition, leading to interference with normal haemopoiesis and excessive production of abnormal monoclonal antibodies (paraprotein). The activation of osteoclasts in the surrounding bone tissue exposes to the risk of pathological fractures and hypercalcemia [2-4]. Molecular imaging modalities such as fluorine-18- fluorodeoxyglucose positron emission tomography (FDG-PET) or positron emission tomography/computed tomography (FDG-PET/CT) have emerged recently as reliable methods in the initial staging and treatment planning of patients with MM. FDG is a glucose analogue which accumulates into cells in proportion with their glycolytic activity: therefore, high-metabolism neoplastic cells show an increased FDG uptake in comparison with normal surrounding tissue. Standardized Uptake Value (SUV) is a semi-quantitative estimate of glycolytic activity in neoplastic lesions. The role of FDG-PET and PET/CT in the staging of patients with recent diagnosis of MM has been extensively investigated, with high sensitivity values, especially for the detection of extramedullary lesions [5], whereas Magnetic Resonance Imaging (MRI) performs better to detect intramedullary sites of disease [6]. Besides, FDG uptake allows to distinguish between non-active and metabolically active lesions, thus playing an important prognostic role: in fact, lesions showing higher FDG uptake are probably growing more rapidly than lesions which show low or no detectable uptake at all [7]. Less known is the role of this nuclear medicine technique in the treatment response monitoring in patients with MM. Conventional Whole-Body X-ray Survey (WBXRS) and MRI often do not show any significant changes in myelomatous lesions after treatment, even in case a good response has been achieved; furthermore, changes in lesion size and/or signal intensity on MRI are not specific for good response, as they can be seen also in patients with disease progression [8]. Conversely, the metabolic burden of myelomatous lesions as assessed by FDG-PET or PET/CT reflects modifications in glucose metabolism induced by the treatment on tumoral cells, thus becoming the earliest evaluation of response [8,9]. However, false-positive post-treatment findings can be seen even on FDG-PET, due to bone marrow reconversion after therapy or necrosis-induced inflammation in sites of good response [10]. A recently published review on this topic [11] has showed that at least ten papers, either prospectively or retrospectively conducted, have studied the role of FDG-PET or PET/CTin the posttreatment evaluation of patients affected by MM. This nuclear medicine method has revealed to be reliable in distinguishing metabolically active lesions from inactive ones and to assess post-treatment decrease in FDG uptake within previously detected high-metabolic lesions, as a sign of good response. Obviously, a baseline FDG-PET or PET/CT scan is mandatory as comparator to assess the treatment response at posttreatment examination. Besides, there is a clear advantage with FDGPET or PET/CT compared to other diagnostic tools, such as MRI: the former provides a more accurate whole-body coverage with a single scan, not allowed by MRI. That is why FDGPET or PET/CT is useful in detecting additional lesions in almost 30% of patients previously diagnosed with apparently solitary plasmacytoma [12]. FDG uptake in sites of good response decreases far before than morphological changes on WBXRS or MRI can be evident, since functional changes assessed by FDGPET usually precede morphological changes evaluated by conventional imaging method. Negative findings on post-treatment scan are therefore well correlated with complete clinical and histological remission or, at least, low risk of recurrence or disease progression; conversely, persistence of metabolically active lesions is related to shorter overall and eventfree survival. Therefore, post-treatment FDG-PET findings could be of higher prognostic significance than standard response monitoring methods. As demonstrated by Sager et al. [13], post-treatment changes in metabolic burden of myelomatous lesions significantly correlate with the degree of bone marrow cellularity and plasma cell ratio. Moreover, a significant positive correlation was found between the presence of FDG-avid focal lesions and the evidence of monoclonal paraprotein and/or increased serum gamma globulin fractions and free light chains. Stratification of prognosis is of great relevance in patients affected by MM, since the assessment of the risk of recurrence allows a more accurate patient management and increases the overall survival. Whereas conventional techniques like MRI are helpful to define the number and site of lesions, as well as the pattern of bone marrow involvement, FDGPET or PET/CT adds the concept of the degree of metabolic activity, which is a reflector of the aggressiveness of neoplastic cells: a negative FDGPET pattern is a favourable prognostic factor, especially in patients with high-risk MM [14-16]. However, to date, the response to treatment using FDG-PET or PET/CT and the prognostic value of these techniques have been mostly evaluated on a small number of patients with MM and further large and multicentric prospective studies are needed to substantiate the role of FDG-PET or PET/CT in this setting
Author(s):
Carmelo Caldarella
Abstract | PDF
Share this

Google scholar citation report
Citations : 161
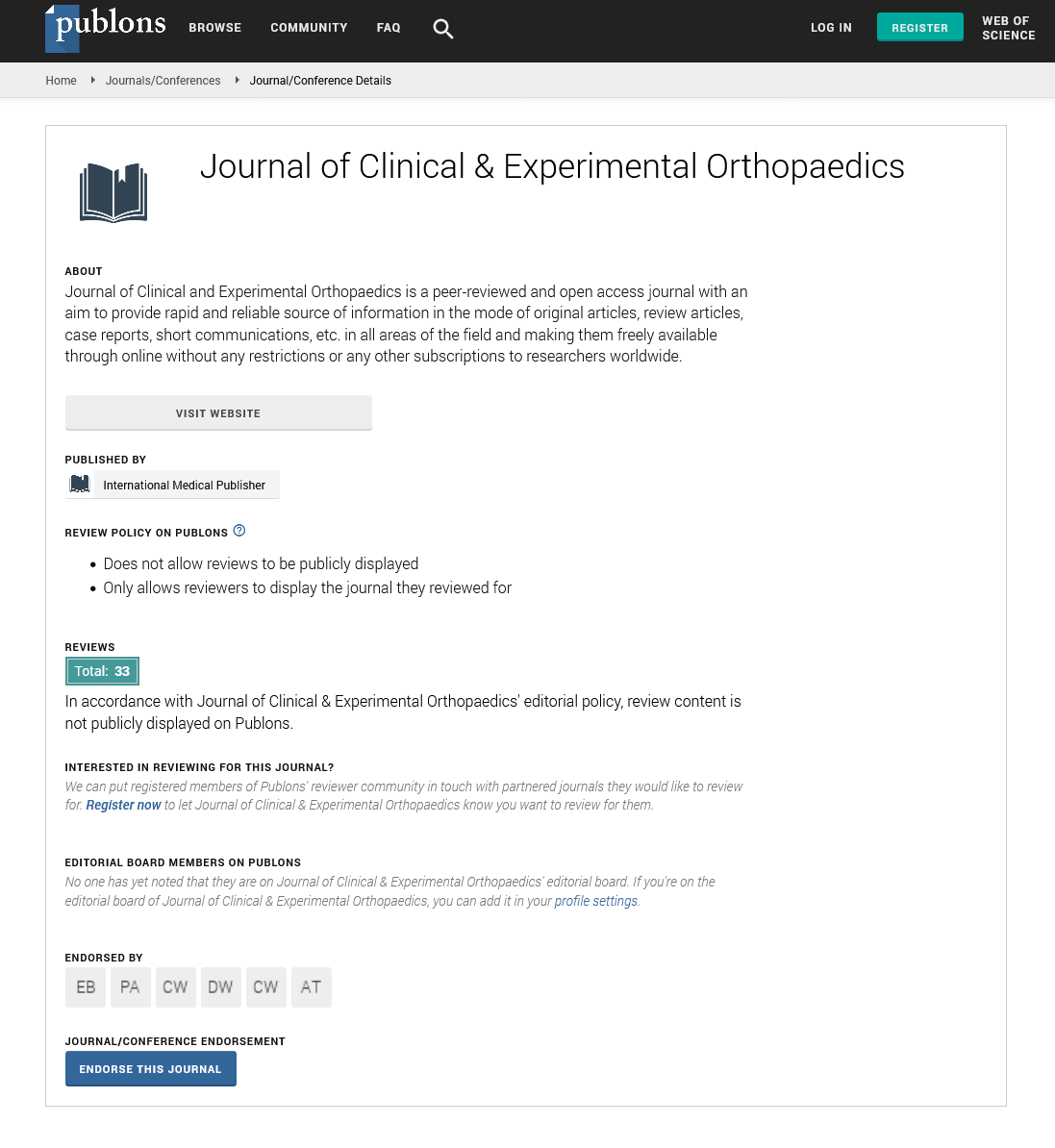
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences