Abstract
Ultrasound-guided ultraminimally invasive carpal tunnel release
Carpal tunnel syndrome is the most surgically treated entrapment neuropathy. It affects 1 million adults in the United States annually. Several studies suggest smaller incisions related to lower rates of scar tenderness, pillar pain rates and earlier return to work. Ultrasound-guided ultraminimally invasive release is performed with 1 mm incision, in an ambulant regimen, with local anesthesia, without the need for ischemia. Simultaneous bilateral release is possible even in patients with diseases considered contraindications for classic techniques.
.
The instrument set included long needles (a 16-gauge, 1.7-mm diameter Abbocath, USA), a V-shaped straight curette, a blunt dissector, a hook knife (Aesculap 2,3 mm), and an ultrasound device (Alpinion ECube15) with a 10-17–MHz linear transducer and the Needle Vision Plus™ software package. The patient is placed supine, with the hand on a table and the palm up. We do not use ischemia. We delineate the midpoint between the nerve and the ulnar vessels, trying to define Nakamichi zone´s midpoint. At the selected midpoint at the forearm, we insert a large spinal needle with local anesthesia and check we pierce the deepest fibers and are beneath the transverse carpal ligament. Color-doppler function may help us to safely determine the superficial palmar arch
and guide the distal limit of our instruments. We insert the small and medium V-shaped straight curette guided by the needle. The release starts 2-3 mm proximal to the superficial palmar arch and proximally we extend the release proximal to the pisiform. We remove the hook knife following the curve of the blade so as not to enlarge the incision. The mobility of fingers is immediately checked. No stitches are required. We use adhesive-strips and a padded dressing. The procedure takes 10 minutes
In 20 cadavers we have checked this procedure to be safe, preserving the nerve and vessels and effective. We have operated on 31 hands in 20 patients (11 bilateral cases), 16 women and 4 men. The age ranged from 39 to 74 years. One case was a recurrence of open surgery. Patients required “pain killers” for 1-2 days and returned to activities of daily living or work after 3 days (1-15 days).
The Phalen test, Tinel test, reverse Phalen test, carpal compression test, and grip strength significatively improved. Quick DASH score improved from 57 pre-op (25-89) to 4post-op (0-9). There were no infections nor nerve damage. Minor superficial hematomas were common. Two patients had residual numbness and thenar atrophy despite clinical improvement.
In the clinical series, pain, function and ankle dorsiflexion increased significantly for every patient in the study (mean, 14º;STD 3º). VAS score improved from 7 (6-9) to 0 (0-1) and AOFAS score improved from a mean of 30 (20-40) to 93 (85-100), at 6 months. All athletes returned to their previous sports after 6 months. Superficial hematomas were common in the series and some
patients developed internal hematomas (observed by ultrasound) at the areas of the tendon and muscle surrounding the recession until the third month. There were no instances of over lengthening or Achilles tendon Better outcomes (in terms of pain, strength, function, and cosmetic aspects) have been reported as dissection was
reduced from classic to endoscopic to mini or ultra-minimally invasive approaches. Ultrasound-guided surgery seems to be safe,
helpful and successful for carpal tunnel release. It gives the surgeon direct control of the main structures. Since they can be performed
on an outpatient basis under local anesthesia and without a tourniquet, complications and contraindications are minimized. As it
causes minimal pain and swelling, recovery is quicker..
Author(s):
Manuel Villanueva
Abstract | PDF
Share this

Google scholar citation report
Citations : 161
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
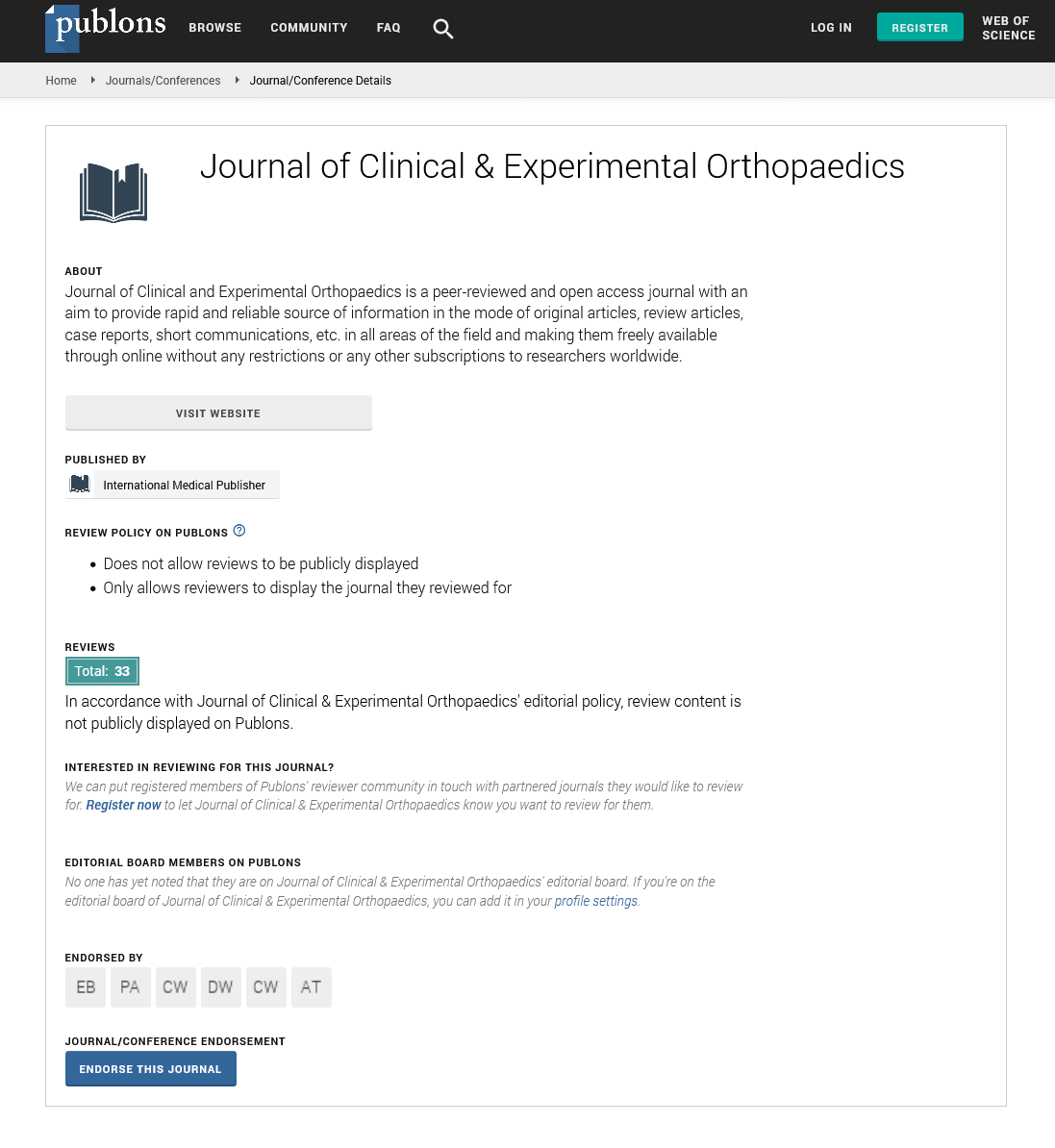
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences