Abstract
Urinary Retention after Orthopedic Surgery: Identification of Risk Factors and Management
Urinary retention is a common complication of post-surgery and anaesthesia and is commonly known as Post-operative Urinary Retention (POUR). The risk of retention is especially high following anorectal surgery, hernia repair, and orthopedic surgery and increases with advancing age of the patient. Many factors are thought to contribute to the development of POUR including traumatic catheterization, pre-existing urologic pathology, and increased fluid requirements of surgery combined with the use of analgesics, opiates and components of anaesthesia The regular capacity of the bladder ranges between 400-600 cc, with the first signal of micturition occurring when the bladder capacity is at 150 cc to the feeling of fullness when to capacity reaches 300 cc. The sensation of fullness occurs at a certain level of afferent activity. Once the voluntary signal to begin voiding has been issued, neurons in pontine micturition centre fire maximally causing the wall of the bladder to contract via the stretch receptors in the bladder. Consequently, the parasympathetic neurons are activated leading to the contraction of the detrusor muscle and relaxation of the bladder neck resulting in micturition. Hindrance to these pathways can accelerate the likelihood of developing POUR. Conservative measure are needed to assist the patient to pass urine, else the bladder will need to be drained using either an intermittent catheter or an indwelling urethral catheter. While there exists little information concerning the outcome of retrospective studies on POUR, this particular review sheds new light on the management strategies and risk factors for the development of POUR after orthopedic surgery to prevent the long-term consequences of this complication.
Author(s):
Anat Zelmanovich* and Debra L. Fromer
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 161
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
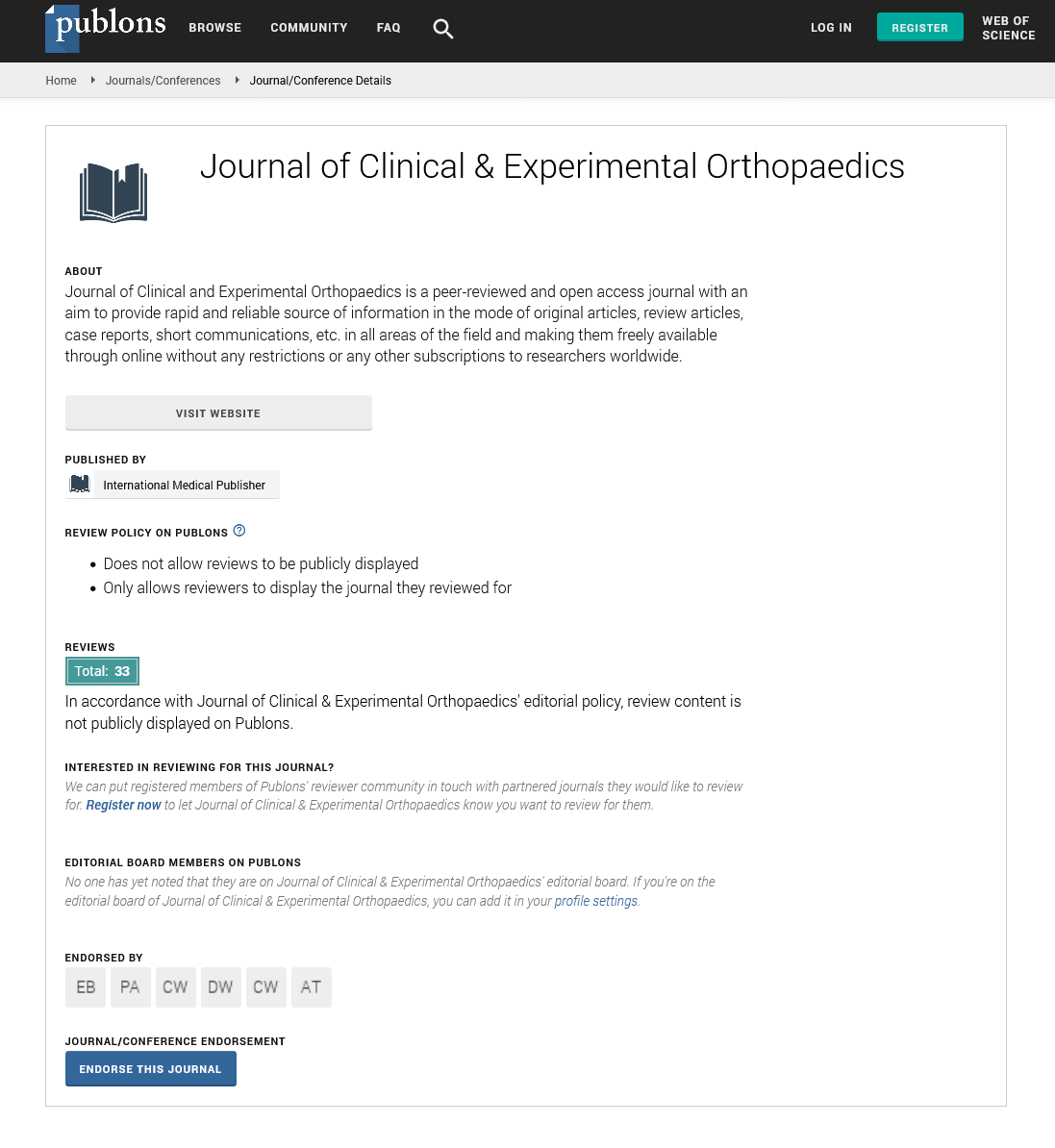
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences