Abstract
Von Hippel-Lindau Syndrome Imaging
Von Hippel–Lindau (VHL) disease is a rare, autosomal dominantly inherited multisystem disorder characterized by development of a variety of benign and malignant tumors. The spectrum of clinical manifestations of the disease is broad and includes retinal and central nervous system hemangioblastomas, endolymphatic sac tumors, renal cysts and tumors, pancreatic cysts and tumors, pheochromocytomas, and epididymal cystadenomas. The most common causes of death in VHL disease patients are renal cell carcinoma and neurologic complications from cerebellar hemangioblastomas. The various manifestations can be demonstrated with different imaging modalities such as ultrasonography, computed tomography, magnetic resonance imaging, and nuclear medicine. Although genetic testing is availabl e, the manifestations of the syndrome are protean; therefore, imaging plays a key role in identification of abnormalities and subsequent follow-up of lesions. It is also used for screening of asymptomatic gene carriers and their long-term surveillance. Screening is important because the lesions in VHL disease are treatable; thus, early detection allows use of more conservative therapy and may enhance the patient’s length and quality of life. A multidisciplinary team approach is important in screening for VHL disease. Von Hippel–Lindau syndrome (VHL) is a hereditary tumor syndrome, arising owing to germline mutations in the VHL tumor suppressor gene, located on the short arm of chromosome 3. VHL is an autosomal dominant disorder, with a prevalence of around one in 36 000 and one in 50 000 live births Around 80% of patients with VHL inherit the disorder from an affected parent, while it may arise de novo in 20%. The mean age of initial tumor diagnosis in VHL is 26 years (range, 1–70 years). The disease is rare with an estimated prevalence of 1:35,000-50,000. Most patients are diagnosed with their first tumor in early adulthood (mean age at diagnosis of initial tumor is 26)
ClassificationVHL can be classified according to clinical phenotypes, and the classification correlates with particular genotypes
Type1: low-risk for pheochromocytoma but higher-risk for
CNS hemangioblastoma, RCC, pancreatic cyst, and pNET
Type2A: High-risk for pheochromocytoma; low-risk for RCC
Type2B: High-risk for pheochromocytoma and RCC
Type2C: High-risk for pheochromocytoma only
Screening The following tests are recommended [2] for screening of abdominal lesions: sonography yearly, beginning at 11 years old; CT yearly or every 2 years, beginning at 20 years old;. MRI or metaiodobenzylguanidines canning as indicated; and determining the level of urinary catecholamines yearly or every 2 years, beginning at 2 years old. Radiation dose is of concern in these patients, who have frequent follow-up studies, and sonography or MRI is preferable
Conclusion The diagnosis and treatment of VHL syndrome is currently relatively difficult. It poses a substantial threat to patients and their families. The early and timely diagnosis and treatment of VHL syndrome can improve patients’ prognosis and rates of survival.
Author(s):
Divya Karavadi
Abstract | PDF
Share this

Google scholar citation report
Citations : 161
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
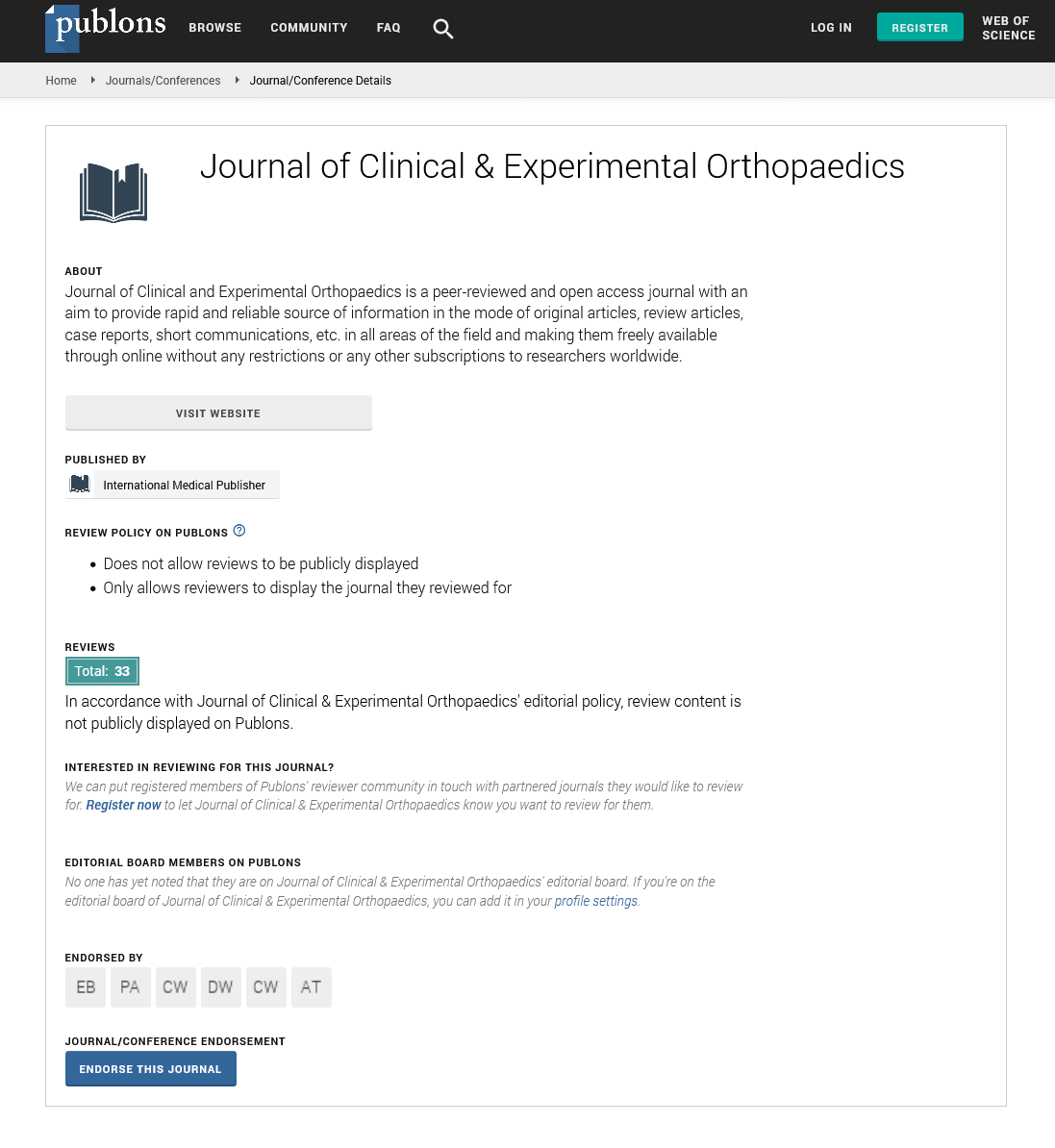
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences