Abstract
what ails our hip replacement surgery peri-operative care system? A comprehensive evaluation of peri-operative mortality in hip arthroplasties at a tertiary care centre
Introduction: With improved survivorship more comorbid elderly patients are being operated for hip arthroplasties. Worldwide all-cause 30-day and 1-year mortality in hip arthroplasties ranges 7-9% and 21-30% respectively, the cause of which remains obscure. The scarcity of mortality data in our country led to systematic effort with aim of evaluating perioperative mortalities in hip arthroplasties, determining better fixation method and reducing avoidable mortalities.tt Materials & Methods: 252 consecutive patients (133 males and 119 females, mean age 58.68years) operated for hip arthroplasties (cemented and uncemented THR and bipolar) were observed prospectively over two years. Heart-rate, O2 saturation and BP were recorded at specific surgical steps and post-operatively for 48 hours. Post-operative Trop-T and 2D Echocardiography were done in all patients and D-Dimer and CTPA in indicated ones. Every postoperative death was extensively studied. Results & Discussion: Majority (63%) were operated for traumatic indications. 48% belonged to ASA grade-1, 46% grade-2 and 4% grade-3. There was statistically significant association of diagnosis (p=0.00241) i.e. traumatic etiology, ASA grade 2(p=0.00163), raised Trop-T (p=0, chest pain and breathlessness (p=0), raised D-Dimer (p=0.04109) and pulmonary embolism (0.00119) with mortality. Mortality rate in our study at post-op 48 hours was 5.5%, 30 day- 8% and one year mortality rate was 19%. No intra operative deaths were noted. With regard to death we obtained a 1-year follow-up of 100%. Out of 14 deaths, 10 were traumatic etiology and 4 non traumatic. There were 8 deaths (out of 14 deaths-57.14%) out of 127 cemented (6.29%) and 6 deaths (out of 14 deaths-42.86%) among 125 uncemented arthroplasties (4.80%). There was no statistically significant association (0.07947) of type of surgery (cemented or uncemented) with mortality. Conclusions: Selection of implant (cemented or uncemented) made no difference in eventual mortality. Cardiovascular complications have overtaken pulmonary emboli as the leading cause of death after hip replacement. Orthopaedicians with anaesthetists must individually evaluate high-risk patients (with cardiovascular and respiratory co-morbidities); intensive monitoring for 48 hours post-operatively and final decision must be made with best interests of the patient paramount
Author(s):
Abhinav Jogan
Abstract | PDF
Share this

Google scholar citation report
Citations : 161
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
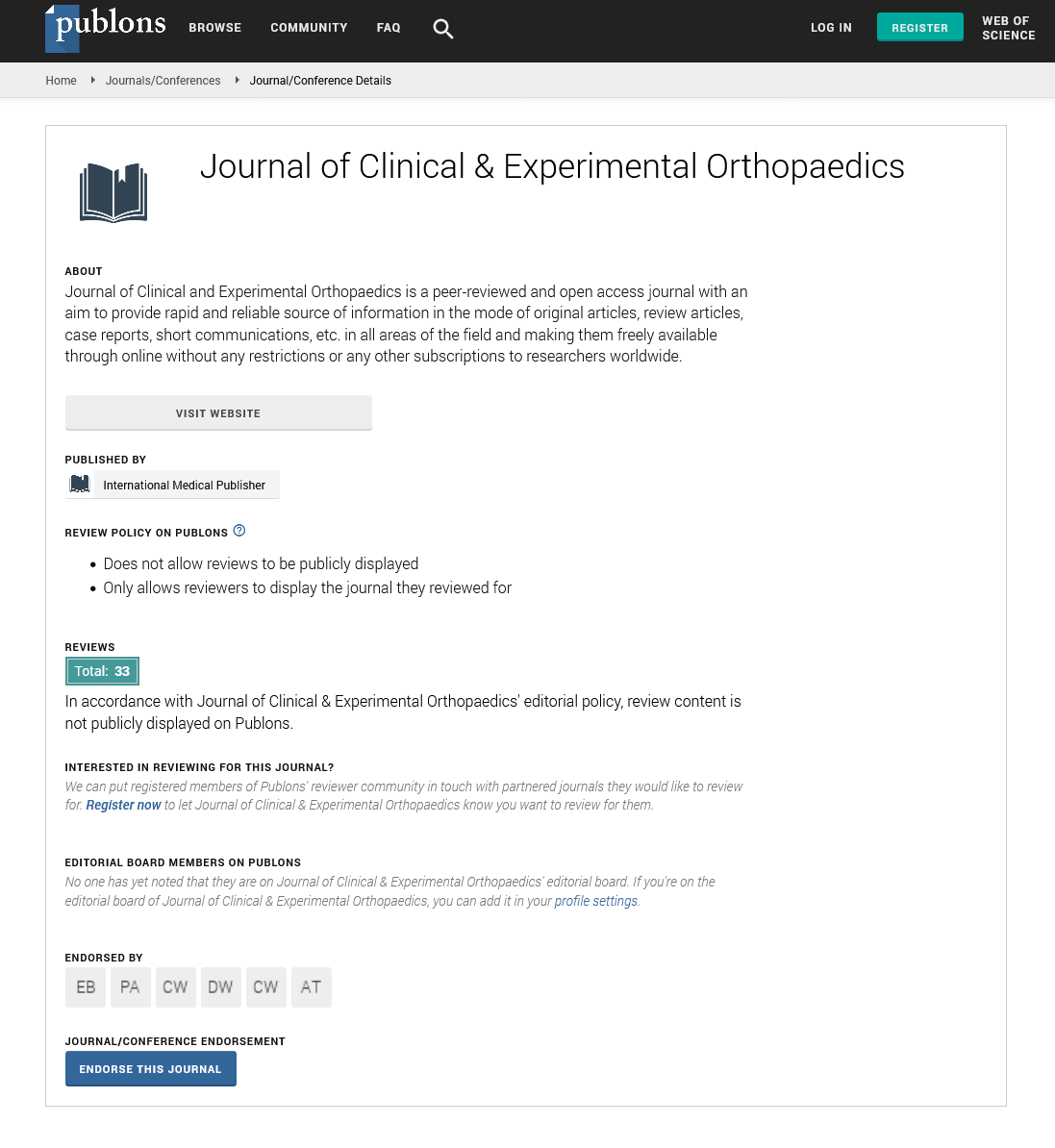
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences