Asymptomatic 3 Proximal Bones Trapezoid and Trapezium Fusion with Hamate Bone Bossing: A Rare Finding as a Case Report
Yogesh Somasundaram*
Department of Osteology, NIMS University, Rajasthan, India
- *Corresponding Author:
- Yogesh Somasundaram
Department of Osteology,
NIMS University,
Rajasthan,
India,
Email: sryogesh22@gmail.com
Received date: March 01, 2023, Manuscript No. IPJCEOP-23-14333; Editor assigned date: March 03, 2023, PreQC No. IPJCEOP-23-14333 (PQ); Reviewed date: March 14, 2023, QC No. IPJCEOP-23-14333; Revised date: March 24, 2023, Manuscript No. IPJCEOP-23-14333 (R); Published date: March 31, 2023, DOI: 10.36648/24718416.9.3.175
Citation: Somasundaram Y (2023) Asymptomatic 3 Proximal Bones Trapezoid and Trapezium Fusio with Hamate Bone Bossing: A Rare Finding as a Case Report. J Clin Exp Orthopr Vol.9 No.3: 175.
Abstract
We report an asymptomatic carpal coalition in a 17 year old male who presented in our outpatient department with an alleged history of fall one day before. He had developed acute pain around the wrist joint following the injury. There was no history of pain in the wrist before the injury. After examination and radiograph revealed the presence of trapezoid and trapezium bony fusion. Carpal coalition of the hand is rare occurrence, which can present as asymptomatic or symptomatic. Carpal coalition can present as bony or membranous. Asymptomatic trapezium trapezoid fusion is reported less in literature.
Keywords
Radiograph; Asymptomatic trapezium; Ligamentous structures; Lateral X-ray
Introduction
Asymptomatic local bone resorption of the tibia under the baseplate can sometimes be observed after Total Knee Arthroplasty (TKA). Its circumstance is not well documented, and so far no explanation is accessible. We report the incidence of this finding in our practice, and investigate whether it can be attributed to particular mechanical factors. The radiographic substitutes of 85 bone ingrowth femoral prostheses in 77 asymptomatic patients were evaluated. The average postoperative follow up time was 21.8 months [1].
In decreasing order of frequency, the alterations are involved as:
• Remodeling of the proximal medial edge of the cut femoral neck (stress shielding) (98%)
• Linear lucency with a thin sclerotic margin at the prosthesis bone interface (that may increase in width or length with time) (79%)
• Endosteal sclerosis at the prosthesis tip (36%)
• Heterotopic bone (24%)
• Cortical thickening at the tip of the prosthesis (12%)
• Prosthetic subsidence (7%)
• Intraoperative fracture (7%)
• Periosteal reaction (4%)
In this investigation, radiographic evidence of these findings was not connected with clinical failure [2]. This is in contrast to the findings in cemented prostheses, in which many of these circumstance (especially the expansion of increasing width of the lucent line adjacent to the cement or prosthesis) have been associated with failure. Long term investigations of porous coated prostheses are required. Currently, however, an awareness of the radiographic alterations that happen with asymptomatic bone ingrowth prostheses can block their misinterpretation as abnormal [3].
Case Presentation
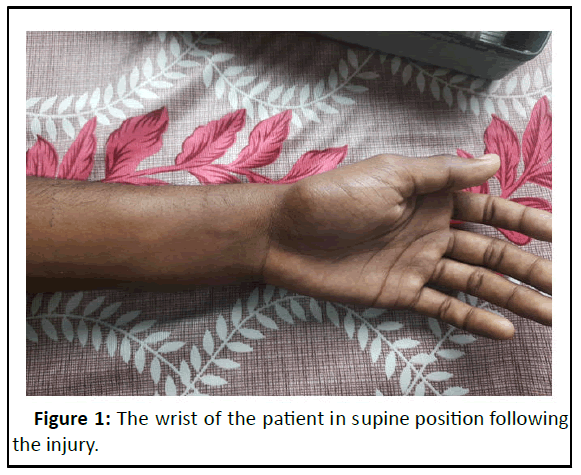
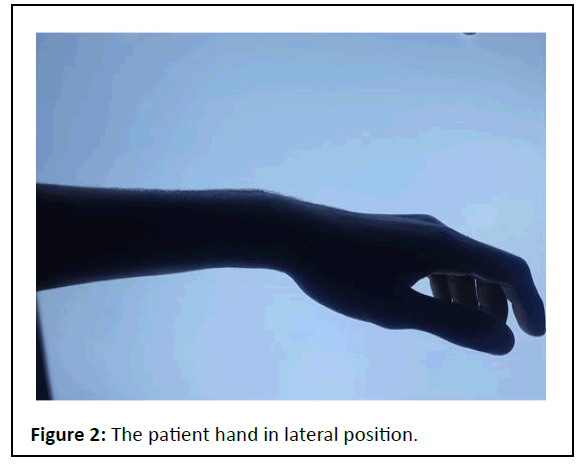
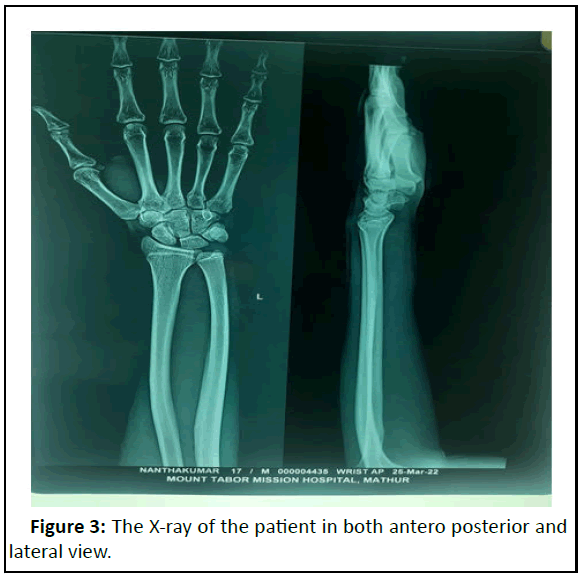
17 year old male with history of fall during riding a bike presented with pain around the wrist joint. There was no effusion/swelling. Past history revealed as no pain and swelling. There was no restriction of wrist joint movement before the incident as compared to other side. There is no history of arthritis, trauma or surgical fusion of the wrist [4,5]. A distal radius fracture was initially thought before the radiograph and Xray done. Anteroposterior and lateral X-ray didn’t show any fracture. On close observation it was found that 3 carpal bones in proximal rows and bossing of proximal hamate bone. The osseous fusion of trapezoid trapezium was found radiographically [6].
Results and Discussion
Patient was given analgesics, ice compression and elevation for 5 days. The pain was reduced and he was able to carry on his daily activities. In one week follow up he reported no pain in wrist joint. Carpal coalition of trapezoid trapezium can be associated with syndromes. But on through investigations of clinical and family history no other significant finding was known. The association with other syndrome was not found in our case. The development of carpal coalition occurs congenitally due to the non formation of demarcation in cartilaginous precursors [7]. In their study emphasized that it is not due to the fusion of carpal bones. In acquired carpal coalition there is an history of multiple inflammatory arthritis, any trauma induced leads to the changes in fibrous, ligamentous structures between the carpal bones leading to coalition. Acquired bony coalition is trauma or surgically fused carpal bones. The origin of the carpal coalition is thus summarized [8].
Importance of radiological identification of carpal coalition may suggest any underlying syndrome, notably fetal alcohol syndrome, turner syndrome and many others. Asymptomatic and isolated fusions are non-syndrome [9,10]. Asymptomatic or mild symptomatic coalition are managed conservatively syndrome carpal coalition are operated surgically to fuse them. Good results have been obtained by surgical fusion for symptomatic carpal coalition (Figures 1-3).
Conclusion
The presence of carpal coalition and the importance of its presence in management of asymptomatic patient are emphasized. The presence of carpal coalition and the importance of its presence in management of asymptomatic patient are emphasized. Local bone resorption of the proximal tibia can happen after TKA and might be attributed to a stress shielding effect. This FE study exhibits that the medial periprosthetic region of the tibia is more sensitive than the lateral region to mediolateral positioning of the baseplate. Medial cortical support of the tibial baseplate is essential for normal stress transfer to the underlying bone. The absence of medial cortical support of the tibial baseplate may lead to local bone resorption at the proximal tibia, as a result of the stress shielding effect. The presence of a complete layer of cement can decrease stress shielding, though. Despite the fact that the local bone resorption is asymptomatic and non progressive, surgeons should be aware of this circumstance in their interpretation of follow up radiographs.
References
- DeFazio MV, Cousins BJ, Miversuski Jr RA, Cardoso R (2013) Carpal coalition: A review of current knowledge and report of a Single institution's experience with asymptomatic intercarpal fusion. Hand 8: 157-163.
- Garn SM, Burdi AR, Babler WJ (1976) Prenatal origins of carpal fusions. Am J Phys Anthropol 45: 203-207.
- Lau GTY, Athalye Jape G, Amery N (2019) Tarsal carpal coalition syndrome: Importance of early diagnosis. BMJ Case Rep CP 12: 229391.
- Duran S, Baskan BM (2015) Coalition of trapezoid capitate and metacarpal: A case report. Acta Orthop Traumatol Turc 49: 698-700.
- Knezevich S, Gottesman M (1990) Symptomatic scapholunatotriquetral carpal coalition with fusion of the capitatometacarpal joint report of a case. Clin Orthop Relat Res 251: 153-156.
- Alemohammad AM, Nakamura K, El-Sheneway M, Viegas SF (2009) Incidence of carpal boss and osseous coalition: An anatomic study. J Hand Surg Am 34: 1-6.
- Das Bhowmik A, Salem Ramakumaran V, Dalal A (2018) Tarsalâ?ÂÃÂcarpal coalition syndrome: Report of a novel missense mutation in NOG gene and phenotypic delineation. Am J Med Genet 176: 219-224.
- Roche AF. (1970) Associations between the rates of maturation of the bones of the handâ?ÂÃÂwrist. Am J Phys Anthropol 33: 341-348.
- Merchant R, Bhatt N, Merchant M (2015) Surgical considerations for massive tarsal coalitions in multiple synostosis syndrome: A case report. Foot Ankle Surg 54: 1162-1165.
- Garn SM, Burdi AR, Babler WJ (1976) Prenatal origins of carpal fusions. Am J Phys Anthropol 45: 203-207.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences