Comparison of Therapeutic Progression Using Anti-Gravity Treadmill for Different Postoperative and Post Injury Conditions
Daniel Savarino and Anna Prunerova
Apex Center for Regenerative Medicine, Tinton Falls, United States
Published Date: 2023-05-22DOI10.36648/2471-8416.9.5.401
Daniel Savarino1* and Anna Prunerova2
1Apex Center for Regenerative Medicine, Tinton Falls, United States
2Head of rehabilitation at Spa Janske lazne, Janske Lazna, Czech Republic
- *Corresponding Author:
- Daniel Savarino
Apex Center for Regenerative Medicine, Tinton Falls,
United States,
E-mail: drsavarino@regeneratenj.com
Received date: April 18, 2023, Manuscript No. IPJCEOP-23-16434; Editor assigned date: April 20, 2023, PreQC No. IPJCEOP-23-16434 (PQ); Reviewed date: May 01, 2023, QC No. IPJCEOP-23-16434; Revised date: May 10, 2023, Manuscript No. IPJCEOP-23-16434 (R); Published date: May 22, 2023, DOI: 10.36648/2471-8416.9.5.401
Citation: Savarino D, Prunerova A (2023) Comparison of Therapeutic Progression Using Anti-Gravity Treadmill for Different Postoperative and Post Injury Conditions. J Clin Exp Orthopr Vol.9 No.5: 401.
Abstract
Background: Rehabilitation of the patient by allowing walking and running with unloaded body weight might represent a solution for shortening immobilization time. The anti-gravity treadmill approach yields a reduction in pain, ground reaction force and lower extremity force during weight-bearing activities and enables patients to engage impaired segments without the need for assistive devices.
Aim: The goal of this clinical trial is to evaluate and compare the progress achieved during anti-gravity treadmill therapy in patients with various musculoskeletal disorders.
Methods: Sixty-nine male and female participants recovering from various musculoskeletal disorders of the lower extremities, who met the study criteria for antigravity treadmill therapy, underwent six twenty-minutes treatment sessions scheduled two days apart. Treatment parameters (speed, inclination and weight loading) were reported during each session and values were used to calculate metabolic rate. The progress achieved between the first and the last treatment was evaluated.
Results: A significant increase in all therapy parameters was observed for all musculoskeletal indications. A comparison between the groups revealed a significant difference in metabolic rate enhancement between postoperative states after total joint arthroplasty and other postoperative/ postinjury states of the lower extremity.
Conclusion: Patients with musculoskeletal disorders of the lower limb experienced significant progress when antigravity treadmill therapy was incorporated in to their rehabilitation protocol. The possibility of partial weight bearing of the damaged limb soon after the trauma enables rapid movement recovery and early discharge to home care.
Keywords
Antigravity treadmill; Musculoskeletal disorders; Arthroplasty; Postoperative/Post-injury rehabilitation; Gait speed; Metabolic rate
Introduction
Musculoskeletal disorders are among the most common causes of disability. In addition to neck and back pain, fractures and other injuries affecting 436 and 305 million patients a year, respectively, constitute a significant part of musculoskeletal diseases [1].
Globally, the number of patients with disabilities is estimated at 15%. Approximately 1.85% of the global populations (131.8 million people) require use of a wheelchair [2]. Assistive devices, such as a wheelchair, crutches or a cane, are not only used by permanently disabled patient, but also patients recovering from injury and/or surgery. As the world’s population ages, the need for medical intervention increases and it is, therefore, crucial to shorten the recovery time. Shortening the immobilization time is also important to facilitate a faster recovery and reduce complications. Immobilization contributes to the degeneration of the immobilized muscles, early joint stiffness, muscle wasting and a decrease in general performance. The longer the immobilization, the longer the course of healing. Therefore, shortening the immobilization time and allowing weight assisted exercise brings the possibility of restoring muscle mass and overall strength of the affected muscle groups, allowing an earlier return to independence in daily activities [3]. Hip and knee arthroplasty are among the most common lower extremity surgeries and with the aging population the number of cases increases yearly [4]. Postoperative precautions focus on the prevention of dislocation rather than on rehabilitation and recovery. It is believed though that immediate postoperative exercise programs might lead to an accelerated functional restoration and faster return to autonomy [5].
Rehabilitation of the patient by allowing walking and running with an unloaded body weight might represent a solution for shortening immobilization time. Such an approach aids in the reduction of pain, ground reaction force and impaired segment force during weight-bearing activities and enables patients to engage impaired segments without the need of assistive devices. An anti-gravity treadmill is a device capable of unloading the body weight while walking and running [6].
Partial-weight bearing therapy performed with the use of an anti-gravity treadmill compared to a standard rehabilitation protocol with the use of crutches showed a significant improvement in leg circumference in patients with tibial or ankle fractures [7].
The benefit of anti-gravity treadmill therapy was further confirmed by multiple studies in patients with other musculoskeletal disorders. Specifically, in patients recovering from injuries of various extent - lower limb fractures, Achilles tendon [8] and Anterior Cruciate Ligament (ACL) rupture [9], pelvis stress injury [10] and lumbar disc herniation [11].
Practically all studies to date have focused on the effect of exercise on the impaired segment in patients with specific disorders. A clinical trial providing comparison of therapy progress in patients with different musculoskeletal injuries was not conducted.
The goal of this clinical trial is to evaluate and compare the progress achieved during anti-gravity treadmill therapy in patients with various musculoskeletal indications. Metabolic rate as a complex indicator of the therapy difficulty represents the primary outcome measure while remaining therapy parameters (speed, inclination and weight loading) will be evaluated as secondary outcomes.
Materials and Methods
The data was reported at the medical spa Janske Lazne between September 2022 and January 2023.
Participants recovering from various musculoskeletal disorders of the lower extremities requiring gait retraining and who met the criteria for the anti-gravity treadmill exercise program were included. The main goal was to improve the patient’s ability to ambulate to the extent of allowing their discharge to home care.
Pregnant, non-cooperative, and those diagnosed with severe cardiovascular disease, epilepsy, bronchial asthma or angina pectoris, acute unstable fracture, severe disc herniation, or increased abdominal pressure were excluded. Before the first exercise session, participants received all information about the treatment program and signed an agreement regarding study participation and possible results publication.
Declaration of Helsinki 1975 ethical guidelines adopted by the General Assembly of the World Medical Association (1997-2000) and by the Convention on Human Rights and Biomedicine of the Council of Europe (1997) were followed in the study design [12].
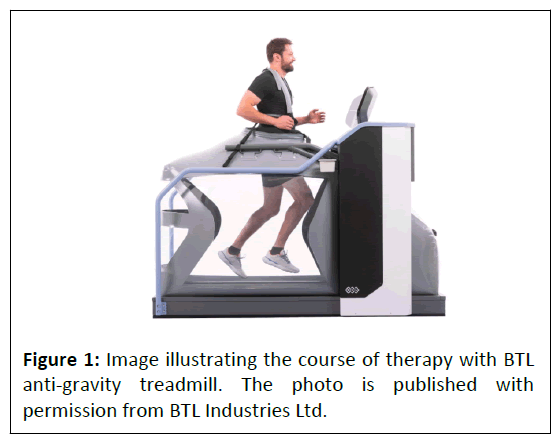
Each patient underwent a treatment program consisting of six twenty-minutes anti-gravity treadmill sessions followed by conventional rehabilitation. During each anti-gravity treadmill session, a gradual increase of treatment parameters (speed, inclination, and weight loading) based on the limitations of each patient was performed (Figure 1).
The anti-gravity treadmill device requires precise setup before each session. To ensure an air-tight enclosure of the lower half of the patient’s body, the treadmill itself is surrounded by an inflatable bag. Once the patient was attached to the bag by shorts with a half zipper, the calibration of the patient’s weight was performed. Next, therapy parameters including speed, inclination and weight unloading were set based on the patient's capabilities. Walking and running at the decreased body weight is ensured and controlled via the adjustable air pressure inside the inflatable bag. Increasing pressure leads to an increase in an upward force offloading the patient’s weight and thus enables incorporating ambulation even in the early stages of recovery when full-weight bearing activities are usually not recommended [13,14].
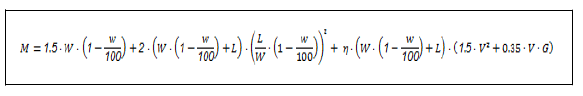
The metabolic rate was calculated based on the achieved therapy progress by the adjusted Pandolf equation [15]. Treadmill inclination (G), walking speed (V) and patient’s weight (W) lowered by the portion unloaded by the anti-gravity treadmill (w) was included in the calculation. As the treadmill surface was considered, the terrain factor (η) was determined to be 1.0 and carried load (L) equaled 0 as there was no additional load during the exercise.
Treatment parameters defining the patient’s progress were further analyzed and evaluated as secondary outcome measures. Speed, inclination and weight unloading were recorded during each session and comparison between the first and the last exercise was performed [16,17].
Using modified equations to calculate metabolic rate makes mutual comparison with the results of similar research complicated and estimates of sample size inaccurate. Therefore, gait speed parameter in patients with different musculoskeletal disorders [18,19] estimated that at least 31 patients would give 80% power to detect a statistical significance (p<0.05).
The script designed for data processing and visualization purposes was created in Matlab (R2010b, Mathworks, Inc., Narick, MA, USA). As the Shapiro-Wilk test revealed non-normal data distribution, non-parametric tests were further used for analysis of statistical significance (Wilcoxon sign rank test) and between-group comparison (Mann-Whitney U test). Due to nonnormal distribution, data were presented as median with Interquartile Range (IQR). Value P<0.05 was considered significant.
Results
A total of 69 patients (aged 62.85 ± 12.11) with various musculoskeletal disorders were enrolled. The majority of participants (81%) were after total joint arthroplasty (aged 69.14 ± 6.77) while the remaining patients (19%) experienced musculoskeletal injury or surgery in the lower extremities (aged 47.54 ± 14.73). The study was generally well tolerated with no adverse events reported.
Metabolic rate
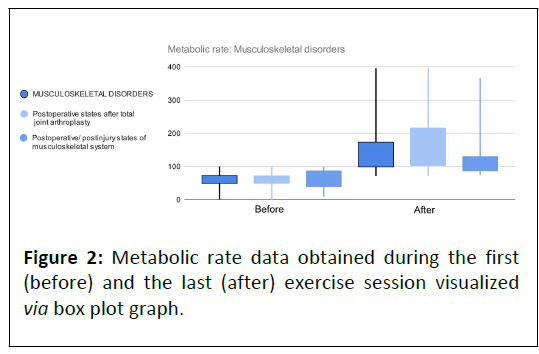
Significant progress in metabolic rate was recorded in all groups however, patients in the total joint arthroplasty group experienced significantly higher improvement than those in other postoperative or post injury states of the lower extremity (Table 1).
| No of patients | Wilcoxon P (0.05) | Metabolic rate before | Metabolic rate after | Improvement | |
|---|---|---|---|---|---|
| Musculoskeletal disorders | 69 | <0.001 | 61.06 (20.35) | 129.65 (71.36) | 113% |
| Postoperative states after total joint arthroplasty | 56 | <0.001 | 61.89 (19.29) | 136.43 (109.93) | 119% |
| Other postoperative/postinjury states of the lower extremity | 13 | <0.001 | 58.14 (44.26) | 103.28 (39.19) | 78% |
| Between-indication group Mann-Whitney P (0.05) | Postoperative states after total joint arthroplasty vs Other Postoperative/ postinjury states of the lower extremity | 0.848 | 0.017 | ||
Table 1: Evaluation of the metabolic rate parameter during the course of the study for individual patient groups, including betweengroup comparisons, using the Mann-Whitney test. Data are displayed as median (IQR) in units W.
Significant enhancement of metabolic rate during the clinical trial and statistically significant difference between indications groups is visible in Figure 2.
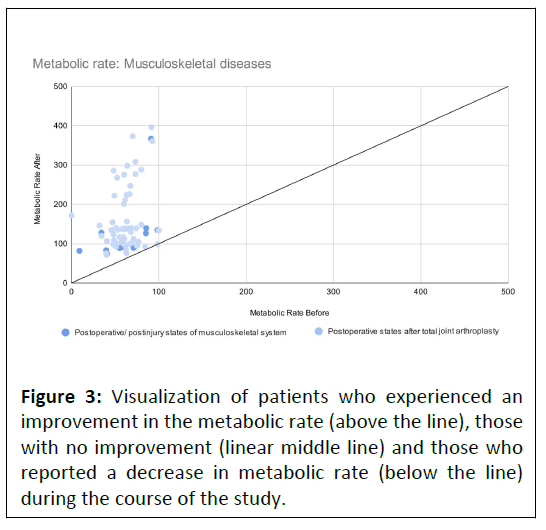
All but one patient reported progress during the course of the study. A single patient recovering after total joint arthroplasty experienced no difference in achieved metabolic rate during the exercise (Figure 3).
Speed
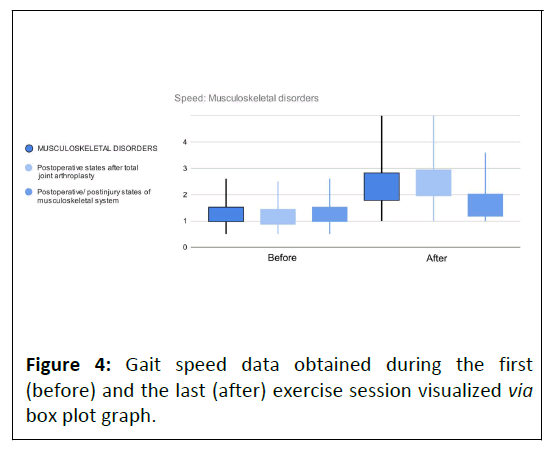
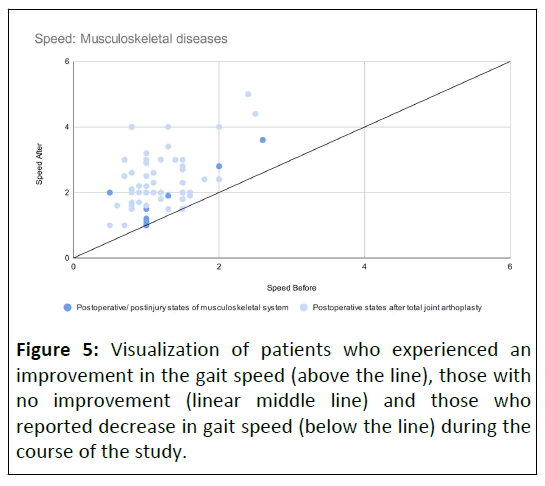
Significant progress in gait speed was recorded in both groups. Again, patients recovering after total joint arthroplasty experienced significantly higher improvement than those in other postoperative or postinjury states of the lower extremity (Table 2).
| No of patients | Wilcoxon P(0.05) | Speed before | Speed after | Improvement | |
|---|---|---|---|---|---|
| Musculoskeletal disorders | 69 | <0.001 | 1.00 (0.50) | 2.00 (1.00) | 100% |
| Postoperative states after total joint arthroplasty | 56 | <0.001 | 1.00 (0.53) | 2.20 (0.95) | 120% |
| Other postoperative/postinjury states of the lower extremity | 13 | 0.004 | 1.20 (0.50) | 1.90 (0.80) | 58% |
| Between-indication group Mann-Whitney P (0.05) | Postoperative states after total joint arthroplasty vs Other postoperative/ postinjury states of the lower extremity | 0.284 | 0.034 | ||
Table 2: Evaluation of the gait speed parameter during the course of the study for individual patient groups, including between-group comparisons, using the Mann-Whitney test. Data are displayed as median (IQR) in units km/h. The device allows setting a minimum speed value of 8 km/h and a maximum value of 25 km/h.
While mutual between-group comparison revealed significant difference in after data, before data are without statistical difference (Figure 4). Out of all study participants, one patient from each indication group did not experience a significant improvement in the gait speed during the rehabilitation program (Figure 5).
Inclination
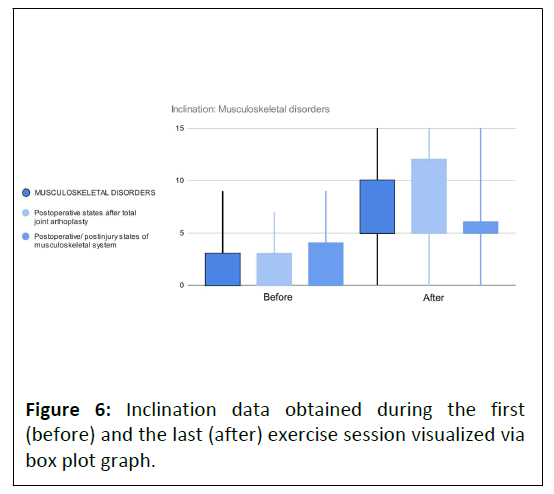
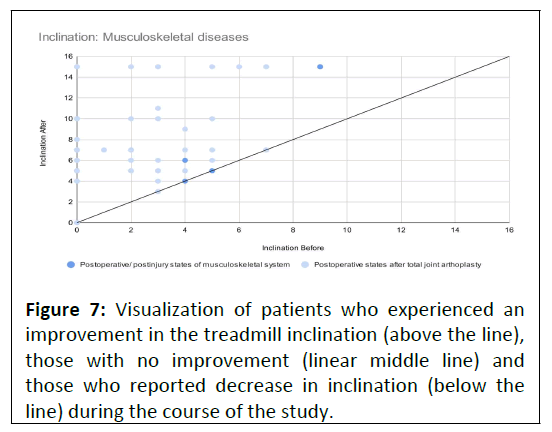
Both indication groups achieved significant progress in treadmill inclination (Table 3). More significant improvement was reported by patients recovering after total joint arthroplasty than those in other postoperative/postinjury states of the lower extremity. A between-group comparison confirmed significant differences in after data while before data did not show significant dissimilarity. This can be visually assessed in Figure 6 displaying before and after data distributions for individual indications groups.
| No of patients | Wilcoxon P(0.05) | Inclination before | Inclination after | Improvement | |
|---|---|---|---|---|---|
| Musculoskeletal disorders | 69 | <0.001 | .00 (3.00) | 7.00 (5.00) | 50% |
| Postoperative states after total joint arthroplasty | 56 | <0.001 | .00 (3.00) | 7.00 (7.00) | 50% |
| Other postoperative/postinjury states of the lower extremity | 13 | 0.005 | .00 (4.00) | 5.00 (1.00) | 150% |
| Between-indication group Mann-Whitney P (0.05) | Postoperative states after total joint arthroplasty vs other Postoperative/ postinjury states of the lower extremity | 0.899 | 0.013 | ||
Table 3: Evaluation of the inclination parameter during the course of the study for individual patient groups, including betweengroup comparisons, using the Mann-Whitney test. Data are displayed as median (IQR) in %. The device allows setting an inclination within the range 0-15%.
Four patients left the treatment program without experiencing progress in treadmill inclination. They were equally distributed between the indications groups (Figure 7).
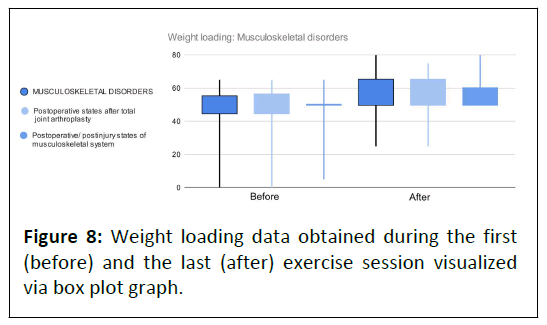
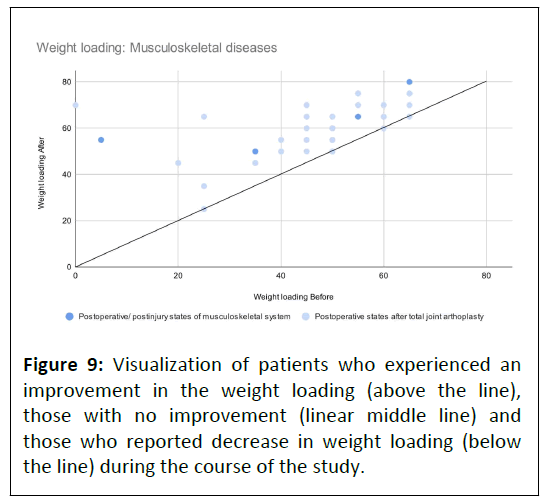
Weight loading
Overall, the least amount of progress was recorded in the weight loading parameter (Table 4). Even so, it was evaluated as statistically significant for both indications groups. Despite the clearly higher improvement in patients after total joint arthroscopy, the difference compared to patients after other surgery/injury of the musculoskeletal system did not reach statistical significance.
| No of patients | Wilcoxon P(0.05) | Weight loading before | Weight loading after | Improvement | |
|---|---|---|---|---|---|
| Musculoskeletal disorders | 69 | <0.001 | 50.00 (10.00) | 65.00 (15.00) | 30% |
| Postoperative states after total joint arthroplasty | 56 | <0.001 | 50.00 (11.25) | 65.00 (15.00) | 30% |
| Other postoperative/postinjury states of the lower extremity | 13 | 0.013 | 50.00 (0.00) | 55.00 (10.00) | 10% |
| Between-indication group Mann-Whitney P (0.05) | Postoperative states after total joint arthroplasty vs other Postoperative/ postinjury states of the lower extremity | 0.82 | 0.224 | ||
Table 4: Evaluation of the weight loading parameter during the course of the study for individual patient groups, including between-group comparisons, using the Mann-Whitney test. Data are displayed as median (IQR) in %. The device allows setting a weight loading parameter within the range 0%-100%.
Similar before and after data distribution for both indications groups was visually confirmed by (Figure 8). During the rehabilitation program, all but four participants experienced progress in the weight loading parameter (Figure 9). Patients with no improvement were all recovering after total joint arthroplasty.
Discussion
This is the first trial monitoring progress using an anti-gravity treadmill exercise protocol and providing mutual comparison between two musculoskeletal indication groups. The study took place in a spa facility providing rehabilitation programs for patients recovering after surgery or injury of the lower extremity. As the patients were in the early recovery stage, the healing process did not allow full weight bearing in the course of the study. Fractures and other musculoskeletal post injury/ surgery conditions require a healing period during which it is not recommended to overload the extremity. Hence, the remaining treatment parameters including speed and inclination were increased prominently in order to achieve locomotion enhancement.
Results reaching statistical significance were reported for all anti-gravity treatment parameters and metabolic rate calculated using adjusted Pandolf equation [15]. This is in accordance with Webber, et al., investigating impact of weight supported treadmill in patients after total knee arthroplasty [18] and Luo, et al., conducting similar research in patients after anterior cruciate ligament reconstruction [19]. Both studies proved significant increase in gait speed during a treatment course. The existing clinical evidence includes multiple studies focusing rather on parameters assessing the extent of musculoskeletal disability than therapy progress [7-11]. However, if we accept that the therapy progress leads to a reduction in the disability of the lower limbs, we can consider the findings of the current study to be completely consistent with the results of previous trials on patients with lower limb fractures [7], Achilles tendon [8] and Anterior Cruciate Ligament (ACL) rupture [9], pelvis stress injury [10] and lumbar disc herniation [11].
Inter-group comparison revealed significant differences between patients recovering after total joint arthroplasty and those in other postoperative/postinjury states of the musculoskeletal system for metabolic rate, speed and inclination.
A simple explanation for the statistically significant mutual comparison of the progress achieved during the exercise could be a marked difference in the mean age of participants among the two groups. Patients recovering after total joint arthroplasty were more than two decades older than the other post injury or surgery patients. This age difference is well aligned with published statistics from US hospitals stating the average patient age for knee arthroplasty is 67 years, hip arthroplasty is 66 years and after other lower limb impairments requiring hospitalization is 47 years [16]. However, the age difference between the two indications groups surprisingly contradicts the results obtained in the present study. Despite the fact that the post arthroplasty group consisted of elderly patients, it achieved significantly better results.
Another possible explanation may be the difference in the recovery time of different musculoskeletal disorders. In a study conducted by Karas, et al., patients post hip or knee arthroplasty self-reported time of recovery between 1 and 5 months while those recovering from tendon/ligament repair stated a period from 1 to 12 months [17]. This finding is consistent with published information for patients considering knee surgery. After total knee replacement, the return to normal activities is relatively quick, while after Anterior Cruciate Ligament (ACL) reconstruction surgery recovery takes a comparably longer time and limits the patient for up to a year [20,21]. A longer recovery period is due to an almost unlimited return to sports activity after an ACL. Patients with an artificial joint must avoid some activities putting an excessive load on the operated knee such as jumping, rapid pivoting and contact sports in general [21]. The long recovery time after ACL can be simply caused by the healing time of the ligament, which requires the longest time of all tissues of the musculoskeletal system [22].
Current study limitations include significantly different ratio of patients with individual indications, absence of a control group enabling a better assessment of achieved progress, lack of parameters determining healing of impaired segments and missing follow up. Measurement tools providing more accurate metabolic rate estimates could replace calculation from available therapeutic parameters. Even though absolute values might be considered inaccurate, for the purpose of mutual between-indications groups’ comparison, relative values are sufficient.
Despite aforementioned shortcomings, the study can be considered beneficial as it is the first to compare the progress achieved during anti-gravity treadmill therapy in patients with different musculoskeletal indications. In the future, it would be appropriate to expand this study with other musculoskeletal disorders such as coxarthrosis, gonarthrosis in the outpatient care, osteoporosis, arthrosis, arthropathy and others.
Conclusion
Patients from both indication groups reported significant progress during an anti-gravity treadmill therapy exercise protocol. Participants recovering after total joint arthroplasty experienced significantly greater improvement than those in other postoperative/postinjury states of the lower extremity. Rehabilitation involving fully or partially weight supported exercises can contribute to the improvement of the patient's movement abilities without excessive load and the risk of damage to the injured segment which can potentially lead to earlier discharge into home care and autonomy in patients’ daily activities.
References
- Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, et al. (2021) Global estimates of the need for rehabilitation based on the global burden of disease study 2019: A systematic analysis for the global burden of disease study 2019. Lancet 396: 2006-2017.
[Crossref], [Google Scholar]
- Wheelchair Foundation (2022) Wheelchair needs in the world.
- Henkelmann R, Schneider S, Muller D, Gahr R, Josten C, et al. (2017) Outcome of patients after lower limb fracture with partial weight bearing postoperatively treated with or without anti-gravity treadmill (alter G®) during six weeks of rehabilitation-a protocol of a prospective randomized trial. BMC Musculoskelet Disord 18: 104.
[Crossref], [Google Scholar], [Indexed]
- Pritchard MG, Murphy J, Cheng L, Janarthann R, Judge A, et al. (2020) Enhanced recovery following hip and knee arthroplasty: A systematic review of cost-effectiveness evidence. BMJ Open 10: e032204.
[Crossref], [Google Scholar]
- Goeb YL, Krell EC, Nguyen JT, Carroll KM, Jerabek SA, et al. (2021) Early recovery outcomes in patients undergoing total hip arthroplasty through a posterior approach with modified postoperative precautions. J Arthroplasty 36: 2817-2822.
[Crossref], [Google Scholar], [Indexed]
- Sueyoshi T, Emoto G (2018) The effect of anti-gravity treadmill on balance in acute phase of post-operative knee rehabilitation. Asian J Sports Med 9: e59287.
[Crossref], [Google Scholar]
- Henkelmann R, Palke L, Schneider S, Muller D, Karich B, et al. (2020) Impact of anti-gravity treadmill rehabilitation therapy on the clinical outcomes after fixation of lower limb fractures: A randomized clinical trial. Clin Rehabil 35: 356-366.
[Crossref], [Google Scholar], [Indexed]
- Saxena A, Granot A (2011) Use of an anti-gravity treadmill in the rehabilitation of the operated achilles tendon: A pilot study. J Foot Ankle Surg 50: 558-561.
[Crossref], [Google Scholar], [Indexed]
- Hansen C, Einarson E, Thomson A, Whiteley R, Witvrouw E (2017) Hamstring and calf muscle activation as a function of bodyweight support during treadmill running in ACL reconstructed athletes. Gait Posture 58: 154-158.
[Crossref], [Google Scholar], [Indexed]
- Tenforde AS, Watanabe LM, Moreno TJ, Fredericson M (2012) Use of an antigravity treadmill for rehabilitation of a pelvic stress injury. PM&R 4: 629-31.
[Crossref], [Google Scholar], [Indexed]
- Moore MN, Vandenakker-Albanese C, Hoffman MD (2010) Use of partial body-weight support for aggressive return to running after lumbar disk herniation: A case report. Arch Phys Med Rehabil 91: 803-5.
[Crossref], [Google Scholar], [Indexed]
- Council of Europe (1997) Convention for protection of human rights and dignity of the human being with regard to the application of biology and biomedicine: Convention on human rights and biomedicine. Kennedy Inst Ethics J 7: 277-290.
[Crossref], [Google Scholar], [Indexed]
- Stockland J, Russell Giveans M, Ames P (2019) The effect of an anti-gravity treadmill on running cadence. Int J Sports Phys Ther 14: 860-865.
[Crossref], [Google Scholar]
- Vincent HK, Madsen A, Vincent KR (2022) Role of antigravity training in rehabilitation and return to sport after running injuries. Arthrosc Sports Med Rehabil 4: 141-149.
[Crossref], [Google Scholar], [Indexed]
- Pandolf KB, Givoni B, Goldman RF (1977) Predicting energy expenditure with loads while standing or walking very slowly. J Appl Physiol Respir Environ Exerc Physiol 43: 577-581.
[Crossref], [Google Scholar], [Indexed]
- Bang H, Chiu YL, Memtsoudis SG, Mandl LA, Della Valle AG, et al. (2010) Total hip and total knee arthroplasties: Trends and disparities revisited. Am J Orthop (Belle Mead NJ) 39: 95-102.
[Crossref], [Google Scholar], [Indexed]
- Karas M, Marinsek N, Goldhahn J, Foschini L, Ramirez E, et al. (2020) Predicting subjective recovery from lower limb surgery using consumer wearables. Digit Biomark 4: 73-86.
[Crossref], [Google Scholar]
- Webber SC, Horvey KJ, Yurach Pikaluk MT, Butcher SJ (2013) Cardiovascular responses in older adults with total knee arthroplasty at rest and with exercise on a positive pressure treadmill. Eur J Appl Physiol 114: 653-662.
[Crossref], [Google Scholar], [Indexed]
- Luo Y, Shen W, Jiang Z, Sha J (2016) Treadmill training with partial body-weight support after anterior cruciate ligament reconstruction: A randomized controlled trial. J Phys Ther Sci 28: 3325-3329.
[Crossref], [Google Scholar], [Indexed]
- Train it right (2021) Knee replacement vs ACL reconstruction surgery.
- van Thiel G (2023) ACL surgery vs total knee replacement surgery.
- Cambridge Osteopathy (2018) How long will this take? Time frames of tissue healing.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences