Gout the Great Mimicker: A Case Report
Omar A Mahroq*, Mujeeb M Shaik and Sarah H Almaged
Department of Orthopedic Surgery, Thumbay University Hospital, Ajman, United Arab Emirates
Published Date: 2023-12-15DOI10.36648/2471-8416.9.5.402
Omar A Mahroq*, Mujeeb M Shaik and Sarah H Almaged
Department of Orthopedic Surgery, Thumbay University Hospital, Ajman, United Arab Emirates
- *Corresponding Author:
- Omar A Mahroq
Department of Orthopedic Surgery,
Thumbay University Hospital, Ajman,
United Arab Emirates,
E-mail: dromarmahroq@gmail.com
Received date: November 14, 2023, Manuscript No. IPJCEOP-23-18126; Editor assigned date: November 17, 2023, PreQC No. IPJCEOP-23-18126 (PQ); Reviewed date: December 01, 2023, QC No. IPJCEOP-23-18126; Revised date: December 08, 2023, Manuscript No. IPJCEOP-23-18126 (R); Published date: December 15, 2023, DOI: 10.36648/2471-8416.9.5.402
Citation: Mahroq OA, Shaik MM, Almaged SH (2023) Gout the Great Mimicker: A Case Report. J Clin Exp Orthopr Vol.9 No.5: 402.
Abstract
Gout stands as the prevailing form of inflammatory arthritis, arising from the accumulation of uric acid crystals within the joints. This accumulation results in the emergence of intense pain, noticeable swelling and joint stiffness. Although it most commonly targets the first metatarsophalangeal joint, gout can exert its effects on various other joints throughout the body. We present a unique case of 38 year old male presenting with right knee intraarticular synovial mass and also presenting with another soft tissue swelling on nasal bridge. He underwent investigations including MRI Knee reported as synovial hemangioma, CT scan reported as chondroma of nasal bone. He had surgical excision of both lesions and biopsy of both lesions confirm the diagnose of gouty tophus.
Keywords
Gout; Tophi; Pseudogout; Synovial hemangioma; Chondroma
Introduction
Gout, the most prevalent form of inflammatory arthritis, has been the subject of extensive research worldwide, elucidating the well-established risk factors contributing to its onset. Yet, what makes gout intriguing is its proclivity to mimic various other medical conditions, making the diagnosis elusive. Some studies have even dubbed it as "the great mimicker”. While elevated uric acid levels serve as the biochemical culprit, it is noteworthy that some patients fail to develop urate crystals. In fact, approximately 5% of individuals who develop gout exhibit uric acid levels exceeding 9 mg/dL [1]. A study conducted in 2009 reported that among 339 patients presenting with acute gout, 14% displayed serum uric acid levels at or below 6 mg/dL, while 18% fell within the range of 6 mg/dL to 8 mg/dL [2]. Such atypical presentations often involve complications like nephrolithiasis, tophi formation and recurrent acute inflammatory attacks, all of which significantly affect an individual's quality of life.
To underscore the pervasive nature of gout, the musculoskeletal disorders and risk factors expert group, as part of the GBD (Global Burden of Disease) 2010 study, recognized gout as a global health burden [2]. In this context, suboptimal disease management has not only resulted in increased morbidity but also imposes a substantial healthcare utilization and cost burden [2].
Gout, characterized by the deposition of Monosodium Urate (MSU) crystals, predominantly in joint spaces, represents a wellknown type of arthritis. In its early stages, treatment primarily involves the use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) and colchicine. Modern management has evolved to incorporate a multi-faceted approach, combining various therapeutic strategies for prevention, dissolution of urate crystals and targeted therapy. Lifestyle modifications are also an essential component of patient care, aimed at enhancing overall quality of life.
Here we discuss a case of 38 year old male who works as store supervisor with past medical history of hyperlipidemia, hyperuricemia and type 2 diabetes presenting with 2 years history of chronic painful swollen right knee and 2 years history swelling of nasal bone to our institute which ultimately turned out to be gouty tophus at both sites.
Case Presentation
Chief complaint
Our patient is a 38 year old male presented to orthopedic outpatient department with bilateral knee pain and swelling for 2 years. He is also noted to have swelling on the bridge of nose that is non-tender for 2 years. He was referred to ENT for further evaluation.
History of present illness
Patient presented with complaints of recurrent attacks of bilateral knee pain and swelling for two years. There is no preceding history of trauma. His pain is mainly anteromedial aspect of knee and intermittent in nature, worse with climbing stairs. He is unable to perform Muslim prayers on floor.
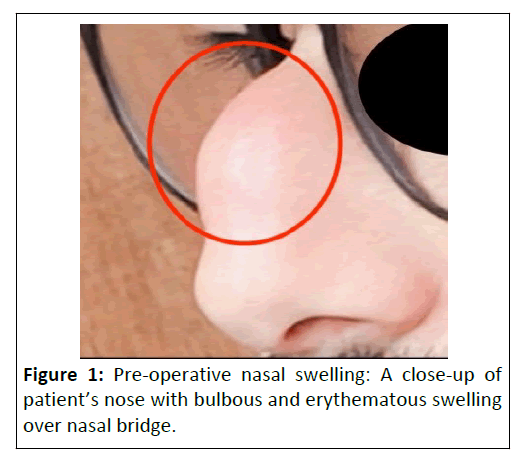
He is also noted to have swelling over nasal bridge for 2 years which is non-tender, but gradually increasing in size in the last one year.
Past medical history
The patient suffers from hyperuricemia, hyperlipidemia and diabetes mellitus. He had recurrent attacks of hyperuricemia with arthalgia for last three years which were treated inadequately, with short courses of alluprinol. He was not on any anti-hyperuricemia medications in the last 6 months prior to his current problem.
However, he is regular with his oral medications for diabetes and hyperlipidemia. He had no past surgical history. He has never smoked in the past and does not consume alcohol.
Clinical examinations
Orthopedic examination: Tender and swollen both knees with moderate effusion in right knee. Crepitus present in patellofemoral movements. Both knee ROM 0-120 degree, tender medial joint lines. There is exquisite tenderness over medial parapatellar tissue. MacMurray test for medial meniscus is equivocal in both knees. Cruciate and collaterals are intact.
ENT clinical examination: A 2 cm firm swelling over middle of nasal bridge which is non-tender. Overlying skin color, turgor and texture are normal. Prominent skin vessels noted over swelling. Minimal nasal mucinous discharge noted (Figure 1).
Pre-op investigations
Hematological investigations: CBC shows that he is anemic and has leukocytosis. High LDL, HDL, HbA1C, ESR, elevated urea, serum creatinine and elevated uric acid levels noted.
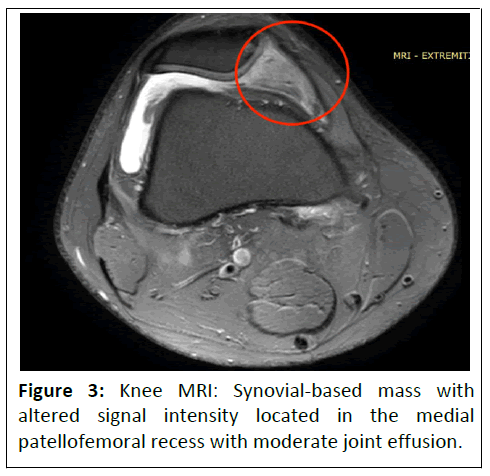
Radiological investigations: X-ray of both knees shows early osteoarthritis changes. Right knee MRI showed early osteoarthritis changes with moderate effusion. There is also a well-defined synovial based mass with altered signal intensity located in the medial patellofemoral recess. Radiological diagnostic possibility of synovial hemangioma considered. Left knee MRI showed early osteoarthritis changes with mild effusion.
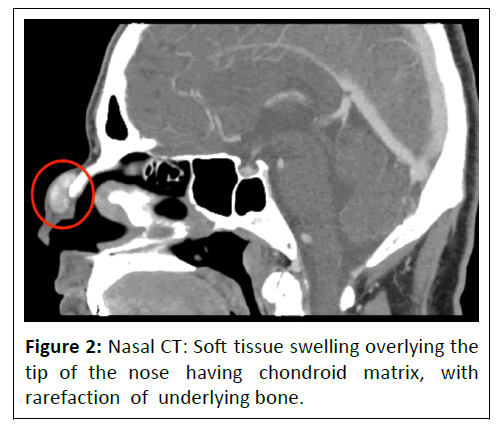
CT scan of maxilla/paranasal sinuses with contrast: Bilateral maxillary sinusitis, deviated nasal septum to the left with nasal spur. A well-defined soft tissue swelling overlying the tip of the nasal bone having chondroid matrix, with rarefaction of the underlying bone-benign etiology like chondroma is considered (Figures 2 and 3).
Preliminary differentials diagnosis
Preliminary differentials were synovial hemangioma of right knee, chondroma of nasal bone and articular cartilage, gouty arthritis and early osteoarthritis of both knees. Synovial hemangioma and chondroma were the initial favored diagnoses due to the radiology reports.
Treatment
Patient was advised surgical excision biopsy of both masses under general anesthesia. Patient was started on febuxostat 80 mg to decrease his uric acid pre-operatively. Patient was operated by both orthopedic and ENT surgical teams successively under same anesthesia.
Right knee arthroscopic excisional biopsy of soft tissue lump in medial parapatellar region by orthopedic team was performed initially followed by excision of nasal mass via external rhinoplasty columellar incision by ENT team was performed under general anesthesia.
Orthopedic surgical findings
During arthroscopic procedure, multiple chalky deposits noted in all three compartments of the knee and meniscal surfaces. Discrete lump of 1 cm × 1.5 cm is seen in medial parapatellar region that was biopsied and excised with arthroscopic shaver.
ENT surgical notes
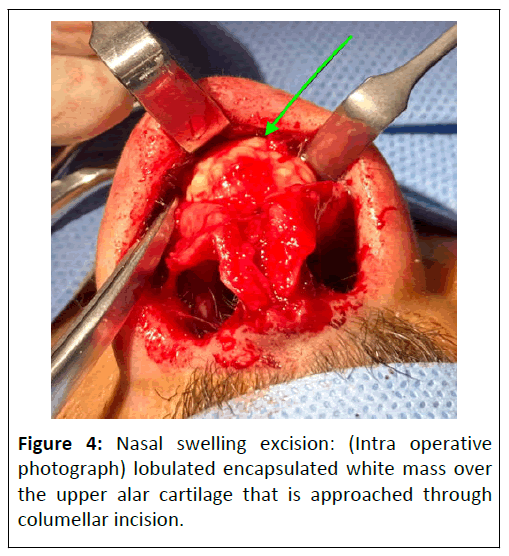
• Nasal bridge mass approached through columellar incision.
• Lobulated encapsulated white mass 1 cm × 1 cm over the upper Alar cartilage, dissected from above and removed.
• Both surgical samples were submitted for histopathological examination.
• Both surgeries had no perioperative complications.
• Post-operatively, active motion of the knee and lower limbs was encouraged.
At 2 weeks follow up wounds of knee surgery and nasal surgery healed well. Patient became completely asymptomatic at both sites. His serum uric acid level returned to normal level and he was advised to continue febuxostat for long term with regular uric acid checks (Figure 4).
Biopsy report
Excision biopsy of synovial tissue and calci ied mass of right knee: Showing eosinophilic material surrounded by giant cell reaction, fibrosis and severe chronic inflammation consistent with gouty tophus.
Nasal excisional biopsy: Showing well circumscribed masses of fluffy amorphous eosinophilic material surrounded by giant cell reaction, fibrosis and severe chronic inflammation consistent with gouty tophus.
Results and Discussion
This case shows how gout can be different and unusual, not always causing bad joint pain as we might expect. Gouty lumps called tophi can make it tricky for doctors at times to know it's gout. For example, lumps in the nose area can make it swollen and drippy, seeming like something else, like a tumor. Swelling in the middle of the knee that might look like a different knee problem could actually be gout and this delay in finding gout might cause more problems, like difficulty moving, as we see in this case.
Gout's prevalence spans from less than 1% to 6.8%, with an incidence rate ranging from 0.58 to 2.89 cases per 1,000 persons. These figures vary based on the specific population under study. Over the past five decades, there has been a noticeable global surge in the burden of gout, highlighting an increased occurrence of this condition worldwide [3].
In 1990, the prevalence of gout was recorded at 20.2 million individuals. Shockingly, this figure more than doubled by 2017, reaching 41.2 million people affected by this condition. Despite significant advancements in gout treatments, the failure to adhere to treatment regimens has contributed to this substantial increase in numbers over the years [4]. Gout stands out as the prevailing cause of inflammatory arthritis among adults, impacting around 1%-2% of the population in industrialized nations. It is notably more prevalent in elderly males. The development of gouty arthropathy is linked to irregular purine metabolism, culminating in the production of uric acid. This condition arises from either inadequate elimination or excessive generation of uric acid, leading to prolonged hyperuricemia. Elevated levels of uric acid, surpassing local solubility thresholds, can prompt the deposition of Monosodium Urate (MSU) crystals within joints, on the surface of hyaline cartilage, and in periarticular soft tissues like tendons, ligaments, retinacula, and bursae. This, in turn, triggers an inflammatory response. While gout predominantly affects peripheral joints, it is noteworthy that the axial skeleton may also be impacted [5]. Numerous risk factors contribute to the development of gout. Genetic mutations affecting the renal urate transporter system might result in either the underexcretion or overproduction of uric acid crystals. This, in turn, can lead to the formation of gout nodules, commonly referred to as tophi. Additional risk factors for gout encompass advanced age, as well as a family or personal history of gout attacks. Conditions like osteoarthritis, the consumption of alcohol, and diets rich in purine-laden foods can also contribute to its development. Moreover, medications such as thiazide diuretics, commonly used for hypertension, might trigger gout in particularly susceptible individuals. Thiazide and thiazide-like diuretics have been linked to an increased risk of gout due to a surge in serum uric acid concentration, typically occurring a few days after the initiation of therapy. Clinically, the features of gout and drug-induced gout often present similarly [6].
The diagnostic challenge of atypical presentation was amplified by unusual radiological appearance that diverted initial clinical suspicion away from gout, despite high serum uric acid levels. However, a comprehensive investigative approach involving imaging studies, multidisciplinary surgical approach and histopathological examination unveiled the elusive nature of gout. Gout was initially excluded from the list of potential diagnoses since the lesions observed in our patient bore a resemblance to synovial hemangioma or chondroma. This illustrates how gout can manifest in unusual ways, mimicking different ailments and delaying accurate diagnosis. This similarity led us to lean toward an idiopathic cause or benign tumor cause. Hence, it is crucial to contemplate the possibility of gout in patients exhibiting multiple joint lesions, even if these lesions are soft, fluctuant and lack the classic appearance of tophi. Excision biopsy of the lesions is of utmost importance for an accurate diagnosis and to support symptomatic relief, as was the case with our patient.
Overall, this case highlights the importance of a multidisciplinary approach in addressing the diverse and atypical presentations of gout. The successful management not only resolved acute inflammation and leukocytosis but also served as a testament to the significance of a unified, collaborative effort in handling such complex gout cases.
Conclusion
Because of irregular and inadequate medical treatment of symptomatic hyperuricemia, our patient developed tophus deposit at multiple sites, this case highlight the important of regular long term treatment of hyperuricemia with regular monitoring of uric acid levels.
Recognizing gout's elusive nature, especially in cases with atypical presentations, emphasizes the necessity for a collaborative approach among medical experts. The successful management of this complex gout case highlights the importance of a unified effort in addressing such challenging scenarios, ultimately ensuring better patient outcomes.
References
- Chen LX, Schumacher HR (2008) Gout: An evidence based-review. J Clin Rheumatol 14: 55-62.
[Crossref], [Google Scholar], [Indexed]
- Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, et al. (2012) Disability Adjusted Life Years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: A systematic analysis for the global burden of disease study 2010. Lancet 380: 2197-2223.
[Crossref], [Google Scholar], [Indexed]
- Abdel-Khalek A, Tariq A, White JA, Cheema AR, Dhillon S, et al. (2023) A typical presentation of gout: A case report. Cureus 15: e36707.
[Crossref], [Google Scholar], [Indexed]
- Hainer BL, Matheson E, Wilkes RT (2014) Diagnosis, treatment and prevention of gout. Am Fam Physician 90: 831-836.
[Google Scholar], [Indexed]
- Weaver JS, Vina ER, Munk PL, Klauser AS, Elifritz JM, et al. (2021) Gouty arthropathy: Review of clinical manifestations and treatment, with emphasis on imaging. J Clin Med 11: 166.
[Crossref], [Google Scholar], [Indexed]
- Gupta A, Rai S, Sinha R, Achar C (2009) Tophi as an initial manifestation of gout. J Cytol 26: 165-166.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences