Intercalary Right Femur Resection , Recycling Autograft , Reconstruction with Vascularized Fibula Graft and Iocking Plate of Right Femur .
Ezieki dar
Ezieki dar*
Department of Kulliyah of Medicine, Internal Islamic University Malaysia
- *Corresponding Author:
- Ezieki dar
Department of Kulliyah of Medicine, Internal Islamic University Malaysia
Tel: 0244508206
E-mail: julliaalba321@gmail.com
Received Date: July 17, 2021; Accepted Date: October 5, 2021; Published Date: October 15, 2021
Citation: Ezieki dar (2021) Intercalary right femur resection, recycling autograft, reconstruction with vascularized fibula graft and locking plate of right femur. Am J Clin Exp Orthop Vol: 7 No:6
Summary
The life expectancy of patients operated for malignant bone tumour has increased, especially with accurate preoperative imaging techniques, early diagnosis and effective chemotherapy. This has resulted in changes to the initial surgical management, with fewer amputations and more limb salvaging surgical options. Femur is a common site of primary bone tumors. Most bone sarcomas occur in the metaphyseal portion of the bone and typical resection involves the whole proximal or distal part of the bone. Therefore, in most cases, the resected segment of bone is replaced by a prosthesis, which provides satisfactory results quickly after surgery.
However, when the tumour involves the diaphyseal portion of the bone, an intercalary reconstruction method is required. The intercalary resection of malignant bone tumour results in a bone defect which can represent a challenge to address. The most commonly used surgical reconstructive options for these defects include allografts, vascularized fibular grafts, autogenous devitalized tumor bearing bone graft, combination of allografts ordevitalized autografts with vascularized fibular grafts, segmental bone transport, bone cement spacer, or intercalary endoprosthesis.
We present a case of reconstruction of intercalary femur defect using a devitalized autograft with combination of vascularized fibula graft. This is an inaugural case performed in Hospital Kuala Lumpur Orthopaedics Oncology Unit, which is the vibrant epicentre of tumour referrals throughout the nation [1].
Case Report
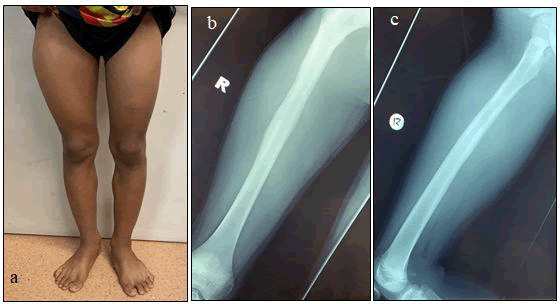
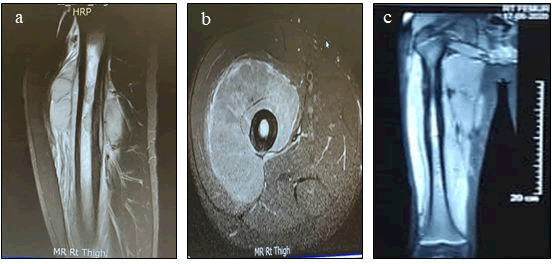
A 14 year old boy presented with right thigh pain and swelling which was significantly increasing in size within 3 weeks duration. Patient had no history of fall or trauma, no evidence of recent infection nor constitutional symptoms and was still able to ambulate without support. Systemic examination were unremarkable apart from right lower limb swelling. MRI of right thigh was done revealing large right thigh anterior compartment poorly marginated heterogenous soft tissue mass encasing proximal and mid right femur measuring 7.8 x 8.3 x 11.7cm (APxWxCC) with cortical involvement and intramedullary lesions.
Subsequently a trucut biopsy of right thigh was performed and microscopically levels show multiple strips of lesional tumour tissue with lobular growth pattern and dark condensed rounded nuclei with no evidence of necrosis leaning towards Ewing’s Sarcoma of right femur. Patient was subjected for neo-adjuvant chemotherapy and a CT staging was done prior to it showing no evidence of distant metastases. Patient subsequently completed an uneventful neo-adjuvant chemotherapy regimen (AEWS0031 Protocol – Compressed VDC-IE) for 5 cycles. MR imaging for reassessment was done upon completion of 3rd cycle of chemotherapy and findings revealed less visible appearance of the intramedullary lesion and significantly smaller soft tissue component of the right proximal femoral lesion associated with vastus intermedius infiltration in keeping with good treatment response [2].
Figure 1: a) Clinical image of bilateral lower limb with marked swelling over anterolateral aspect of right thigh. b) Plain radiograph of Anteroposterior view of right femur c) Plain radiograph of lateral view of right femur showing an onion peel periosteal reaction over midshaft of femur with otherwise intact bone.
Figure 2: MRI images of right femur with contrast a) T2W sagittal view of right femur demonstrating hyperintense signal with intramedullary lesion at proximal diaphysis and associated extensive marrow edema. b) T1W axial view showing a heterogenous soft tissue mass circumferentially encasing proximal aspect of right femur which is isointense to muscle with no involvement of neurovascular bundle. c) T2W coronal view of MRI which was repeated after 3rd cycle chemotherapy revealing reduction of marrow edema involving diaphysis of right femur with no obvious epiphyseal involvement of lesion hence preserving right knee and hip joint.[3-5].
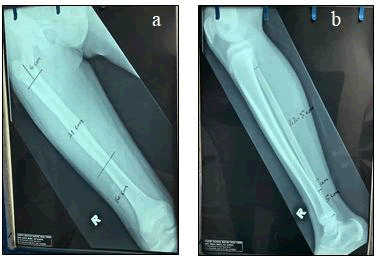
Upon completion of 5th cycle of neo-adjuvant chemotherapy, patient was prepared for Intercalary Resection of right femur with Recycling Autograft, Reconstruction with Free Vascularized Fibular Graft & Locking Compression Plate of femur. Anaesthetics screening prior to surgery was uneventful as patient was passed fit to undergo a major surgery. A thorough pre-operative planning was discussed including measurement of resection length of bones & method of assembling the vascularized fibula graft for reconstruction. [6].
Pre-operative planning
Base on the MRI of right thigh findings, intramedullary lesion are present in the proximal diaphysis collectively measures about 4.4cm in length and associated with extensive marrow edema of the femur.
• The distance between the proximal margins of the intramedullary lesion with the hip joint is about 10.5cm
• The distance between the distal margins of the intramedullary lesion with the knee joint is about 24cm
• The distance between the proximal margins of marrow edema with the hip joint is about 8cm
• The distance between the distal margins marrow edema with the knee joint is about 15cm.
Procedure
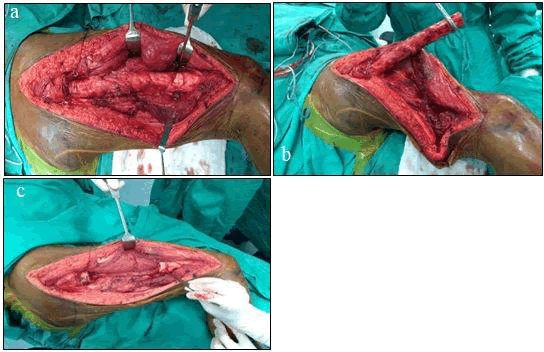
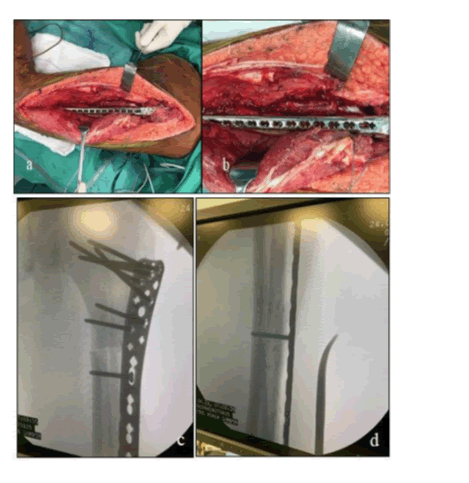
Figure 4: a) Lateral incision was made from tip of greater trochanter until distal third thigh, incision was deepened until iliotibial tract exposed & split. Subvastus approach was used after cut at proximal bone cut level and vastus lateralis muscle tagged. b &c) Wide resection was performed around bone segment, distal bone cut was made approximately 16cm from knee joint line, and proximal bone cut was made just inferior to lesser trochanter. All four perforators were identified and preserved. Both proximal and distal femur medullary canal was reamed up to 14mm to incorporate fibula graft. Resected bone segment was reamed until 11mm using a rigid reamer.
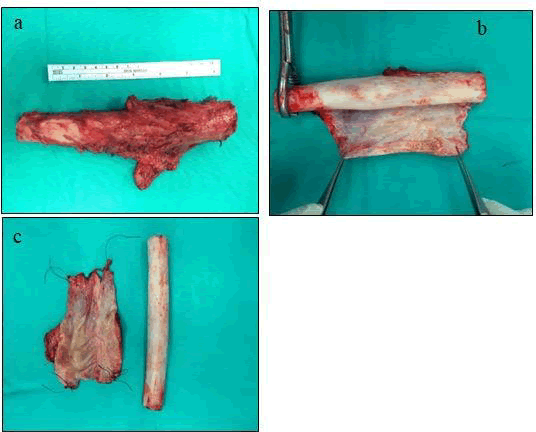
Bone Preparation
Pasteurization
Figure 6: a) Cortex and medullary canal of bone cleaned, curreted and washed with copious amount of sterile water, soaked in 70% alcohol, mixed with Vancomycin 1gram then rinsed with normal saline before pasteurization. b) Anterolateral part of bone segment was then excised with aid of oscillating saw prior to pasteurization. c) A longitudinal groove was created in the cortex of the autograft in a sufficient size to receive the VFG in the medullary canal in a concentric assembly. d) Bone segment & resected anterolateral part of cortex were isolated during pasteurization using plastic wrappers and pasteurized with Normal Saline under 65 degrees for about 40 minutes. Segments were then soaked in Gentamycin 480mg.[7]
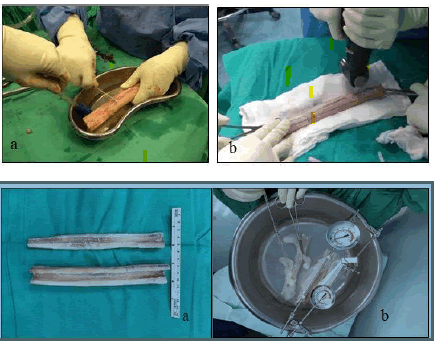
Vascularized fibula graft transfer
Fibula bone with pedicle was harvested from ipsilateral limb by microsurgical team of surgeons using separate instruments to avoid cross contamination. Tibial and peroneal artery were ligated proximal to bifurcation and approximately 24.5cm fibula bone was resected together with its pedicle, no distal tibio-fibula fixation required post resection. Fibula graft was inserted into medullary canal and covered by recycled femur autograft over its posteromedial aspect. Anastomosis of femoral artery and vein to 1st branch of profunda femoris was performed.
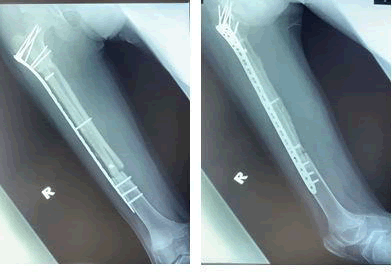
Vascular anastomosis was checked intra-operatively using Doppler scan and demonstrates good flow. Stabilization of construct was achieved via fixation of locking plate positioned over lateral aspect of femur [8].
Figure 7: Images above (a-d) demonstrates fixation of proximal tibia variable angle medial locking plate over lateral cortex of femur. 3.5mm cortical screw was used to lag both bones. The harvested fibula was at least 2 cm longer than the length of the femoral resection in order to allow a minimum overlap of 1cm for each osteotomy.
Vastus Lateralis muscle repair was commenced prior to iliotibial band closure. Deep and superficial drain inserted prior to closure. Patient tolerated surgery well and was transferred to general ward the following day. There were no complications or major difficulties encountered during procedure. Postoperative antibiotics were continued until drains were removed. Controlled passive movements of the hip and knee was encouraged.
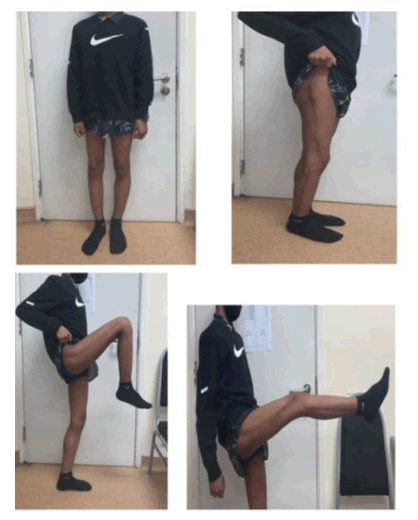
Figure 10: At 6 months follow up there were no limb length discrepancy measured where else marked clinical improvement noticed with good range of movement and a stable gait. Patient was otherwise healthy with well healed surgical wound and was compliant to partial weight bearing with aid of abductor brace. He was then referred to oncology counterpart for continuation of chemotherapy
Discussions
In line with accurate preoperative imaging techniques, early diagnosis and advances in chemotherapy, the survival of patients with a bone sarcoma has greatly improved. Since most patients with a primary bone tumour are young, a long-lasting reconstruction should be the aim of limb salvage surgery. If intercalary resection of malignant bone tumors can be performed with preservation of the adjacent joints, the expected function is superior as the patient’s native joints above and below the reconstruction are left undisturbed.
Reconstruction options following intercalary resection of lower extremity malignancy have included the use of massive allograft, autoclaved autografts, pasteurized autografts, irradiated autografts, and segmental prostheses to name a few. Each procedure has its own shortcomings and no standardized method has been established. One of the main disadvantages of devitalized autografts such as autoclaved, pasteurized, or irradiated autografts is that it takes a long time for them to be revascularized and incorporated into the surrounding bone
Biological reconstruction with a VFG is a reliable method of reconstruction after excision of an intercalary bone tumour from a long bone. Apart from retaining its endosteal and periosteal blood supply, a VFG preserves its biological and mechanical properties, heals by primary union, and can hypertrophy in response to load. The unique shape and size of the fibula allow it to be inserted into the medullary cavity of the femur, where it can be used concentrically with an autograft. It also allows the reconstruction of very large intercalary defects [10].
| Operative techniques | Indication | Advantages | Disadvantages |
|---|---|---|---|
| Allograft | Osteolytic and osteoblastic lesions | Avoids donor site morbidity | Needs bone banks High rates of complications Risk of infectious diseases Transmission |
| Free Vascularized Fibula Graft | Better indicated for areas of lighter stress loads as upper limb, mid shaft tibia, and pediatric patients | Viable graft Doesn’t undergo resorption by creeping substitution | Has small cross-sectional area Weaker than the originally resected long bone Long period of non-weight-bearing Fatigue fracture Donor site complications. Time consuming procedure |
| Combined FVFG and allograft | Large intercalary bone defect | Combine the biological activity of the FVFG with the initial mechanical strength of the allograft | Require bone bank Donor sitecomplications Risk of infectious diseases transmission Lengthy procedure |
| Segmental transport | Indicated mainly in children andinpatients with a long-life expectancy | Regeneration of living bone whichremains permanent once it is found | Time consuming Needs patient’s cooperation Pin tract infection Delayed consolidation Union problems at the docking site Malalignment in large bone defects |
| Operative techniques | Indication | Advantages | Disadvantages |
| Devitalized autografts | Indicated mainly in osteoblastic lesionsor when two thirds of the cortex were preserved | Dimensions of the devitalized autograftprecisely match the host bone No risk of disease transmission or graftrejection Devitalized autograft acts as a scaffold for creeping substitution | Contraindicated in marked osteolyticlesions Impossibility of histological analysis of the whole specimen. |
| Segmental Prosthesis | Metastatic, lymphoma and multiplemyeloma patients Elderly patientsdue to poor healing capacity | Immediate stability Early weight-bearing Rapid rehabilitation | Aseptic loosening Periprosthetic fracture Low survival rates especially in youngpatients |
| Bone cement spacer and induced membranetechnique | Better indicated for lesions of theupper limb | Simple technique The reactive membrane acts as a periosteum, prevents resorption of graft and secretes growth factors | Two stage procedure Difficult application for lower limbreconstruction due to higher stress loads |
Recycling Autograft
Biological reconstruction performed via reuse of the devitalized resected tumor-bearing bone is a viable option. The techniques of devitalizing procedures may include irradiation, autoclaving, pasteurization, or freezing with liquid nitrogen. Reconstruction is performed by re-implantation of the devitalized autograft and stabilization by suitable osteosynthesis.
Major advantages of these procedures are that the reconstruction surgery can be performed more easily as the dimensions of the devitalized autograft precisely match the host bone. There is no risk of disease transmission or graft rejection due to immunological reaction. Moreover, devitalized autograft acts as a scaffold for creeping substitution as the graft is invaded by viable bone tissue with progressive substitution from peripheral adjacent host bone. Potential complications in recycled autografts include nonunion/delayed union, infection, fractures, epiphyseal slip in younger patients, bone resorption, and graft necrosis.
Pasteurized Autograft
Pasteurization was proven to be an effective method for devitalizing the tumor-bearing bone. Pasteurization can kill the malignant cells while the mechanical strength and bone-inducing property of the graft can be preserved. Pasteurization is the technique of heating the resected tumor bone segment at a low temperature (60 C) for 30 min. The superiority of pasteurization technique over other methods of heat treatment such as autoclaving or boiling was proved by previous reports of the literature.
Urist et al. observed that in heat treatment with the temperature greater than 70 C, the biologic activity of the bone morphogenetic protein (BMP), which is essential for bone induction, is completely destroyed. Potential complications of pasteurized autograft include infection, nonunion, fractures, and bone resorption. Jeon et al. reported that the rates of deep infection, bone non-union, and fracture were 14.3%, 23.8%, and 9.5%, respectively. Han et al. reported infection rate of 15%, nonunion rate of 42%, and fracture rate of 23%.
Vascularized fibula graft
Free vascularized fibular graft (FVFG) was firstly reported in 1977 by Weiland et al. for reconstruction of long bone defect after resection of bone tumor. Since then, the FVFG has become a popular biological reconstructive option for limb-sparing surgery after resection of the malignant bone tumors. Vascularized bone grafts don’t undergo resorption by creeping substitution due to their intact vascularity.
FVFG can incorporate into the adjacent host bone directly via bone union similar to the process of healing of fractures. Due to the viability of FVFG, the structural integrity is well preserved until the bony union is achieved. Furthermore, soft tissue structures like skin, fascia, and muscle may be harvested concomitantly with the fibula and used for more complex soft tissue reconstruction.
FVFG can be used in three forms of reconstructive options
Single vascularized fibular graft which is mainly indicated for reconstruction of areas with lighter stress loads as in upper extremity reconstruction, segmental defects of the mid-tibia, and intercalary defects in pediatric patients.
Vascularized double-barreled fibula which can be indicated for areas with intermediate stress loads such as femur and pelvis. This technique can provide the double volume of a fibular graft for the same length of the defect with the same number of the microvascular anastomosis.
In combination with an allograft or devitalized autograft such as pasteurized or irradiated autograft.
Despite these advantages, the fibula has small cross-sectional area and is weaker than the originally resected long bone, particularly the femur. The sufficient fibular thickness to allow full weight-bearing is achieved several years after the surgery as the fibula needs a long time to undergo hyper-trophy through processes of pressure transport, microfractures, and callus formation. Therefore, a long period of non or partial weight-bearing is necessary.
The reported complications include recipient site complications (fatigue fractures of the fibular graft, delayed union/nonunion, infection, loss of flap, and hardware failures) and donor site complications (bleeding, peroneal nerve palsy, contracture of flexor hallucis longus, ankle pain, instability, and/or progressive valgus deformity commonly in children. The allograft or devitalized autograft provides a massive bone stock and early stabilization, whereas the vascularized fibular graft facilitates host-graft union.
Chang and Weber reported 6 primary intercalary reconstructions with composite use of a vascularized fibula graft and an allograft. All of the 6 studied patients (100%) achieved successful bone union, and the mean time until bone union was 6 months (range, 3–8 months). Sugiura et al. reported 15 intercalary reconstructions with composite use of a vascularized fibula graft and a pasteurized autograft. Bone union was achieved in 13 cases (87%) and the mean period until bone union was 13.5 months (range, 7–25 months). Postoperative complications included fractures in 2 patients and infection in another 2. There were no local recurrences.
Krieg et al. reported 13 intercalary reconstructions with composite use of a vascularized fibula graft and an extracorporeal irradiated autograft. Nonunion was found in 16% of host-donor junctions and they required additional surgical procedures.
The median time until primary bone union was 7.5 months at metaphyseal junctions and 11.1 months at diaphyseal junctions. Many tumors of the metaphyseo-diaphyseal regions of long bones can be resected with joint preservation resulting in intercalary bone defects. There are many options for reconstruction of these defects including biological and non-biological techniques. Each of these techniques has its advantages and disadvantages so that every patient should be carefully evaluated and the reconstructive option should be individually selected.
In conclusion, we advocate that a devitalized autograft combined with a vascularized fibula graft is a promising biological alternative for intercalary reconstruction after wide resection of malignant bone tumors of the lower extremity, especially in younger patients for whom longer life expectancy and increased physical activity make fractures and infections more likely. In addition, combination of a recycled autograft with a vascularized fibula graft and rigid fixation with a locking plate may offer a good better outcomes although longer follow-up of a greater number of patients will be required to confirm this [11].
References
- Capanna R, Scoccianti G, Frenos F, et al. What was thesurvival of megaprostheses in lower limb reconstructions after tumorresections.Clin Orthop Relat Res 2015; 473: 820–830.
- Watanabe K, Tsuchiya H, Yamamoto N, et al. Over 10-yearfollow-up of functional outcome in patients with bone tumors reconstructedusing distraction osteogenesis. J Orthop Sci 2013; 18: 101–109.
- Demiralp B, Ege T, Kose O, Yurttas Y, Basbozkurt M.Reconstruction of intercalary bone defects following bone tumor resection withsegmental bone transport using an Ilizarov circular external fixator. J OrthopSci 2014; 19: 1004–1011.
- Gupta S, Kafchinski LA, Gundle KR, et al. Intercalaryallograft augmented with intramedullary cement and plate fixation is a reliablesolution after resection of a diaphyseal tumour. Bone Joint J 2017; 99-B: 973–978.
- S.Takenaka N Araki,T.Ueda, Clinical Outcomes ofOsteoarticular Extracorporeal Irradiated Autograft for Malignant Bone TumorHindawi Sarcoma Volume 2020
- Capanna R, Campanacci DA, Belot N, et al. A new reconstructivetechnique for intercalary defects of long bones: the association of massiveallograft with vascular-ized fibular autograft. Long-term results andcomparison with alternative techniques. Orthop Clin North Am 2007; 38: 51–60.
- Zekry KM, Yamamoto N, Hayashi K, et al. Intercalary frozen autograftfor reconstruction of malignant bone and soft tissue tumours. In Orthop (SICOT)2017; 41: 1481–1487.
- Panagopoulos GN, Mavrogenis AF, Mauffrey C, et al. Intercalaryreconstructions after bone tumor resections: a review of treatments. Eur JOrthop Surg Traumatol 2017; 27(6): 737–746.
- Bus MPA, Dijkstra PDS, Van de Sande MAJ, et al. Intercalaryallograft reconstructions following resection of primary bone tumors. J BoneJoint Surg Am 2014; 96: e26: 1–11
- H. Sugiura, M. Takahashi, K. Nakanishi, Y. Nishida, and Y. Kamei,“Pasteurized intercalary autogenous bone graft combined with vascularized fibula,”Clinical Orthopaedics and Related Research, no. 456, pp. 196–202, 2007.
- Beytemür O, Adanir O, Dinçel YM et al. Clavicle diaphyseal fracture,ipsilateral type 3 acromioclavicular joint dislocation stabilized with doubleplate. Int J Shoulder Surg 2013 ;7: 153
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences