Lower Limb Myxoid Liposarcoma with Distant Metastasis: Report of Two Cases and a Literature Review
Cheng Liu, Jing Chen, Fan Xiong, Weihao Jiang, Qiu Cui, Jun Guo, Yanjun Zeng
DOI10.4172/2471-8416.100012
Cheng Liu1, Jing Chen2, Fan Xiong1, Weihao Jiang1, Qiu Cui1, Jun Guo1 and Yanjun Zeng3*
1Department of Orthopedics, the Affiliated Hospital of Academy of Military Medical Sciences, PLA 307th Hospital, Beijing 100071, P.R.China
2Department of Orthopedics, Second Hospital of Beijing Armed Police Corps, Beijing 100045, P.R.China
3Biomechanics and Medical Information Institute, Beijing, University of Technology, Beijing 100022, P.R.China
- *Corresponding Author:
- Yanjun Zeng
Beijing University of Technology, 100Pingleyuan
Chaoyang District, Beijing 100022
P.R.China
Tel: 8610-67391809
E-mail: yjzeng@bjut.edu.cn
Received date: February 29, 2016; Accepted date: March 22, 2016; Published date: March 25, 2016
Citation: Zeng Y, et al. Lower Limb Myxoid Liposarcoma with Distant Metastasis: Report of Two Cases and a Literature Review. J Clin Exp Orthop. 2016, 2:12 doi: 10.4172/2471-8416.100012
Copyright: © 2016, Zeng Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Liposarcoma, mainly involving the deep soft tissue of limbs and torso, especially lower limbs and retroperitoneum, is the second most common malignant tumour derived from primitive mesenchymal topped by malignant fibrous histiocytoma, accounting for 20% of soft tissue Liposarcoma is divided into five histologic subtypes and three biological types based on WHO classification criteria in 2002: 1) well-differentiated liposarcoma (WDLPS) and dedifferentiated liposarcoma (DDLPS); 2) myxoid liposarcoma (MLS) and round cell liposarcoma (RCLS); 3) pleomorphic liposarcoma (PLS). Among them, MLS is biologically characteristic; especially some patients with extrapulmonary metastases come out with poor prognosis. We hereby retrospectively analyse two MLS cases characterized as extrapulmonary metastases treated in our hospital from June 2007 to October 2015and reviewed related literatures as follows.
Methods: We have retrospectively analysed two cases of MLS with distant extrapulmonary metastases and reviewed related literatures.
Result: MLS is relatively sensitive to radiotherapy and chemotherapy, but the therapeutic outcome does not correlate with radiochemotherapy, the more the round cells and the malignant the myxoid liposarcoma. About 1/3 MLS patients have distant metastasis, with predilection to soft tissue and bone of other parts of body, while the bone scanning is usually negative.
Conclusion: As one subtype of liposarcoma, MLS has many specific biological characteristics, like distant metastasis, and currently regular follow-up examination is needed for timely diagnosis and treatment, but individualized treatment may be the future research direction.
Keywords
Myxoid liposarcoma; Distant metastasis; Extrapulmonary metastasis; Negative bone scan
Case 1:
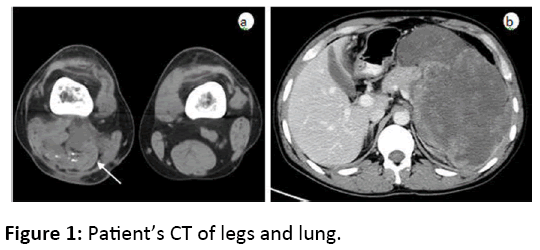
A 31-year-old male patient was hospitalized in our department in January 2010for a distal MLS at right thigh with comprehensive treatment for 2.5 years. A soft tissue mass was found at right popliteal fossa in July 2007 and confirmed as be benign lipoma by biopsy. While the mass gradually enlarged companioned by pain, the patient underwent tumour resection in a local hospital in March 2008 and turned out to be MLS by pathology. Experiencing many unsuccessful conservative treatments, including ethanol and lipiodol injection, interventional chemo-embolization (cisplatin, epirubicin, bleomycin ADM, gelatin sponge, and etc.), HIFU ablation, oral thalidomide and some other anti-tumour treatments, the patient was hospitalized in our department, and a mass around 10 × 12 cm with medium hardness and poor mobility could be palpated in the middle and lower section of back of the right thigh. After 3 cycles of intervention chemotherapy (cisplatin and doxorubicin) through chemotherapy pump placed in right femoral artery, we tried to remove the tumour in May 2010 but found it was surrounded by the sciatic nerve and failed to remove it, thus the amputation was recommended, but it was refused by patient. Pathology diagnosis confirmed to be MLS with a favourable response to chemotherapy. Therefore, 4 cycles of same interventional chemotherapy was performed after surgery, and the last chemotherapy was in November 2010. When the patient felt painful in the left upper abdomen and came back in January 2011, abdominal CT showed a huge left retroperitoneal lesion, confirmed later as metastasis by surgery. The patient died of respiratory and cardiac arrest 3 months after the abdominal surgery. (It was considered that the deep vein thrombosis may result in death, as patient’s family refuse to have autopsy). Patient’s CT of legs and lung are shown in figure 1.
Case 2:
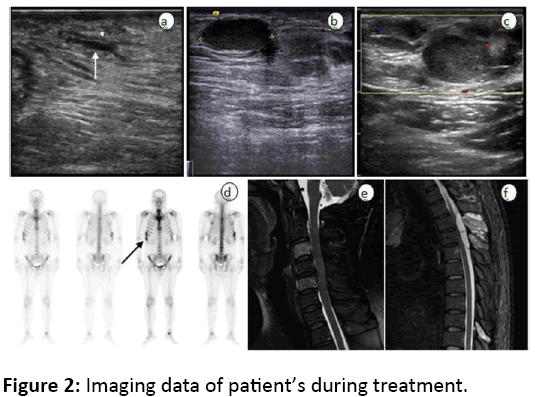
A 30-year-old male patient was hospitalized in our department for recrudescent liposarcoma at the inner side of the right thigh after 3 times surgeries in March 2010. The patient underwent tumour resection and confirmed as MLS by pathology in August 2008, then had wide local excision in September 2008. In August 2009 he had another surgery excision for local relapse in the local hospital with the same pathological results as before. The patient was hospitalized in our department for tumour recurrence in June 2012, and a subcutaneous mass around 2 × 3 cm with medium hardness and poor mobility in the inner side of the right thigh near groin could be palpated. After only 1 cycle of intervention chemotherapy through chemotherapy pump placed in right femoral artery, the patient underwent surgery at local hospital as severe side effects of chemotherapy happened. When the patient hospitalized again in our department for tumour relapse In June 2012, imaging examination showed local recurrence and metastasis at the right inguinal lymph node. After 3 cycles of interventional chemotherapy, wide local excision and metastasis lymph node excision were performed in September 2012, and postoperative pathology confirmed to be MLS with a favourable response to chemotherapy, but the patient refused chemotherapy. In May 2015, the patient was hospitalized again due to numbness and weakness in left upper limb for half a month, and hypaesthesia under the nipple emerged and incomplete paraplegia symptoms developed gradually after hospitalization. C-spine MRI indicated vertebral lesions at C3 and C5 and T-spine MRI indicated an intraspinal space occupied lesion at T3, a softtissue mass at T3 spinous process, and spinous process lesions at T9. Due to rapid aggravation of incomplete paraplegia symptoms, decompressive laminectomy of T3 was performed, and metastasis was confirmed by pathology. In patient’s preoperative bone scan, there is no obvious radionuclide uptake in bones except right rib 7-9, which was later clarified as the results of local trauma two months before bone scanning. The patient refused further treatment after decompressive laminectomy. Four months after surgery, paraplegia symptoms derived from metastasis happened again and eventually he died of multiple organ failure caused by urinary tract infection. Imaging data of patient’s during treatment were shown in figure 2.
Discussion:
Different histologic subtypes of liposarcoma differ at oncobiological behaviours. MLS, accounting for around 30%-55% of liposarcoma, is mainly composed of three substances in histology, including capillary plexus, adipocyte at different developmental stages and mucus matrix rich in mucopolysaccharides. Usually MRI is considered to be the most effective imaging measure for disease diagnosis, however, the degree of tumour differentiation is the key factor to the changes of MRI signal, while the malignancy of MLS would go worse along with the increase of small round cells, and accordingly, MR signals would be uneven with unclear boundary, which is more obvious after enhanced MRI.
Besides, as various kinds of soft-tissue tumours containing mucus-like mesenchyme with complex and overlap pathomorphology, it is difficult in diagnosis. Even it is possible to have false negative diagnosis in biopsy because of the relatively complicated tumour components. Nevertheless, both MLS and RCLS have a same chromosomal translocation t(12;16)(q13;p11), forming a unique TLS / FUS-CHOP fusion gene, therefore specific fusion-gene identification could be applied to identify MLS and RCLS by means of molecular diagnostics.
Like other liposarcoma, surgery is the first choice for MLS, and local radical resection is an effective measure to prevent recurrence and metastasis, but which are both based on explicit diagnosis first. Among 19 such inpatients, except 3 naïve patients, all others have had unplanned excision in other hospital, indicating both diagnosis and treatment of MLS have not drawn enough attention. It is showed that the local recurrence and distant metastasis in patients with unplanned excision are significantly higher than those with radical resection as primary therapy [1], suggesting the importance of primary treatment. Besides, the tumour capsule appears to be complete but, on the contrary, its boundary is actually unclear because of aggressively growing tumour, therefore, it is not uncommon to discover residual satellite lesions after surgery. Just as what happened to our two patients, who suffered from repeated local recurrence after multiple surgeries, and it is estimated to be results of metastasis. But on the other hand, the MLS are often deeply located around major blood vessels or nerves, or wrapped bone tissue; even experienced doctors cannot achieve radical resection, so the prognosis is usually unsatisfactory as well. Besides, these patients usually have relative good limb function, so it is difficult for them to consider amputation. For example, our first MLS case could not underwent wide excision as tumour wrapped sciatic nerve, but he refused amputation, unfortunately he got multiple recurrence and metastasis later. Therefore, it is tough decision for both doctors and patients to choose limb salvage surgery or amputation.
Unlike other liposarcoma, MLS mainly happens in young patients, mostly in limbs, and is relatively sensitive to radiotherapy and chemotherapy, which are often taken as adjuvant treatment. Our treatment is to consider malignant tumour as a systemic disease to take chemotherapy as dominant treatment via arterial infusion chemotherapy, emphasizing local tumour control while taking whole body into account, which has been confirmed to be efficacious in the limb bone and soft tissue tumours [2,3]. Currently doxorubicin and ifosfamide are considered to be effective to MLS. In recent, with the development of molecular diagnosis, drug related gene tests could be applied to analyse whether chemotherapy is effective on liposarcoma in order to have targeted chemotherapy, such as TOP2A, a DNA topoisomerase inhibitor. It was showed in Fountzilas G’s [4] studies that TOP2A expression levels may be a molecular target predicting patients’ sensitivity to anthracycline chemotherapeutic drugs. But it should be clear that even chemotherapy works well on MLS, it does not mean chemotherapy effects correlate with therapeutic outcome just as 2 cases mentioned above, which is different from osteosarcoma [5]. On the other hand, if there are residual lesions during surgery, local postoperative radiotherapy would be a feasible treatment. With the improvement of radiotherapy, intensity-modulated radiation therapy has been applied to MLS patients with multiple metastases who resist chemotherapy. Such method with enhanced target coverage while reduced normal tissues radiation is effective on multiple metastatic lesions [6], indicating the importance of comprehensive treatment of malignant tumours.
MLS’s biological behaviour is related to its cell composition as well. The simple MLS is relatively rare to happened recurrence and distant metastasis, but epigenetic changes would result in cells transforming from simple mucosity to small round cells, together with increased tumour vascular supply, indicating heightened malignance. When the round cells increase to over 5%, the degree of malignancy will significantly increase. It was showed in studies that the prognosis of MLS is closely related to tumour size and patients’ age [7]. When tumour’s size is over 10cm or patient is older than 45, tumour malignancy will increase. Around 1/3 MLS patients would finally have distant metastasis. Compared with other types of limb liposarcoma, MLS is prone to, usually before pulmonary metastases, have metastasis at unusual body parts (such as retroperitoneal, contralateral limb or armpits, etc.), bone (usually vertebra) and etc. MLS metastasis patients often have multiple metastatic lesions, which probably is the results of tumour cell seeding in other locations through blood stream before planting in lung, just, as our first MLS patient whose tumour metastasized to retroperitoneal. By analysing the clonality of different metastatic lesions through molecular biological diagnosis, like RT-PCR, it was confirmed that lesions at other parts are derived from tumour metastasis instead of a second primary tumour so it is necessary to have routine abdominal B ultrasound or CT scan for follow-up MLS patients to rule out possible metastasis. MLS patients with great malignance usually develop bone metastasis, with predilection to spine, nevertheless, the bone scan is often negativejust like our second MLS patient, who was negative on bone scan, but had thoracic and cervical spine metastasis. It is consistent with previous reports, indicating bone scan or PET is not suitable as a mean for follow-up examination. According to the latest hypothesis, the expression of adipophilin and chemokine (CXC motif) receptor 4 (CXCR4) increased in MLS tumour tissues, which is closely correlated with angiogenesis and adiposeness. In addition, Ewing sarcoma breakpoint region 1-DNA damageinducible transcript 3 (EWSR1-DDIT3) fusion transcript is identified to be related with MLS’s bone metastasis, and it selectively repress the osteoblastic activity in the bone metastases, ultimately resulting in negative bone scanning results [8]. It is highly recommended that patients with poorly differentiated MLS should have MRI to scan out bone-related metastasis, especially spinal metastasis.
Researchers are engaging in finding out liposarcoma specific drugs. The mechanisms for the pathogenesis and progress of liposarcoma are better understood with the development of molecular biology. It is demonstrated by in vivo and in vitro studies that FUS-CHOP oncoprotein is an inducer of liposarcoma metastasis due to its transcriptional induction of specific tumour-associated proteases. Advances in liposarcoma research help to further understand liposarcoma on one hand, and orient the targeted therapy for liposarcoma. In Recent, target drug Trabectedin is confirmed to be effective in phase III clinical trial. With the deeper understanding of MLS and improvement of molecular gene diagnosis, accurate diagnosis together with individualized treatment would be the best way out for MLS in the future [9].
References
- Chandrasekar CR, Wafa H, Grimer RJ (2008) The effect of an unplanned excision of a soft-tissue sarcoma on prognosis. J Bone Joint Surg Br. 90:203–208.
- Liu C, Cui Q, Shu C (2013) Comprehensive Treatment Based on Intra-arterial Chemotherapy for Distal Femur Neoplasms. Pathology & Oncology Research19:489-493.
- Guo J, Cui Q, Liu C (2013) Clinical report on transarterialneoadjuvant chemotherapy of malignant fibrous histiocytoma in soft tissue. ClinTranslOncol.15:370-375.
- Fountzilas G, Dafni U, Bobos M (2013) Evaluation of the prognostic role of centromere 17 gain and HER2/topoisomerase II alpha gene status and protein expression in patients with breast cancer treated with anthracycline-containing adjuvant chemotherapy: pooled analysis of two Hellenic Cooperative Oncology Group (HeCOG) phase III trials. BMC Cancer13:163.
- Mullen JT, Hornicek FJ, Harmon DC (2014) Prognostic significance of treatment-induced pathologic necrosis in extremity and truncal soft tissue sarcoma after neoadjuvantchemoradiotherapy120:3676-3682.
- Choi C, Park JH, Lee CG (2015) Successful salvage treatment of myxoid liposarcoma with multiple peritoneal seeding using helical tomotherapy-based intraperitoneal radiotherapy: a case report. BMC Res Notes 8:179.
- Lemeur M, Mattei JC, Souteyrand P (2015) Prognostic factors for the recurrence of myxoid liposarcoma: 20 cases with up to 8 years follow-up. OrthopTraumatolSurg Res. 101:103-107.
- Lin S, Gan Z, Han K (2015) Metastasis of myxoid liposarcoma to fat-bearing areas: A case report of unusual metastatic sites and a hypothesis. OncolLett. 10:2543-2546.
- Manji GA, Singer S, Koff A (2015) Application of molecular biology to individualize therapy for patients with liposarcoma. Am SocClinOncolEduc Book213-218.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences