Multifocal Osteomyelitis in Newborn Child .
George Ezekiel
George Ezekiel
Department of Clinical Orthopaedics international islamic university, Malaysia
- *Corresponding Author:
- George Ezekiel
Department of Clinical Orthopaedics international islamic university, Malaysia
Tel: 175045464
E-mail:ezekielinho85@gmail.com
Received Date: Jul 17, 2021; Accepted Date: October 5, 2021; Published Date: October 15, 2021
Citation: Ezekiel G (2021 Multifocal Osteomyelitis in Newborn Child Am J Clin Exp Orthop Vol: 7 No: 6.
Summary
Osteomyelitis is an infection of the bone and bone marrow that results most commonly from bacteria and mycobacteria. Acute hematogenous osteomyelitis is a rare and easily misdiagnosed infection of the neonatal period and it has the potential to cause life-long musculoskeletal deformities (Steer AC et.al 2004). The incidence of paediatric osteomyelitis varies, but it is usually thought to be uncommon, with a group of researchers estimating a rate of 6.0 per 1000 patients in a children's hospital (Arnold SR et.al 2006). Misdiagnosis is commonly due to unclear signs and symptoms. Delayed treatment can worsen outcome leading to permanent sequalae (Goldman et al 1991). Haematogenous multifocal osteomyelitis in children represents a dangerous form of osteomyelitis in which sepsis can develop quickly if it is not treated early. In this fortunately rare form of the condition, acute infectious foci occur in several bones simultaneously as a result of haematogenous spread. Using appropriate diagnostic measures and intervention, this illness is treatable, with good functional results. We present a rare case of multifocal osteomyelitis in a 4-month-old neonate.
Case report
A baby boy was born at 35 weeks of gestation as the fifth child of both parents. The child was born via an uneventful spontaneous delivery with a birth weight of 2.18 kilogram. Both parents are healthy with no underlying illnesses and there were no maternal, pre-natal and post-natal complications. Mother and child were discharged well from hospital and 3 months later child underwent routine vaccination at nearest health clinic which was given intramuscularly over left thigh [1].
About 5 days after vaccination, child appeared irritable, inactive with had low grade temperature. Parents brought him to a nearby clinic and he was diagnosed with Acute Tonsilitis and a course of Amoxycillin antibiotic was prescribed per orally. Upon completion of antibiotics, parents noted left shoulder swelling which was associated with redness. As a result, there was also reduced movement of affected upper limb. No fall, trauma or any precipitating injuries lead to the new concern. Parents was worried and brought baby to our hospital for further opinion.
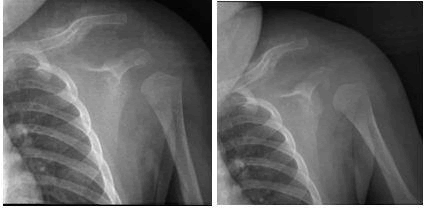
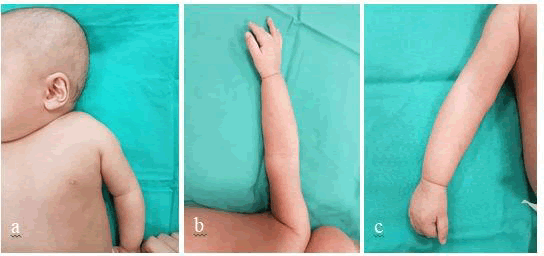
On examination of left shoulder, there was minimal swelling, erythematic changes, and a palpable dense deformity measuring about 2x1cm just over anterior aspect of left clavicle. There were no obvious wound or bruises seen (Fig.1a&b). Child was moving left elbow and wrist joint actively however there was marked reduction of shoulder movement. There were no other significant findings over contralateral upper limb as well as bilateral lower limb. Systemic examination was uneventful. Infective parameters were raised.
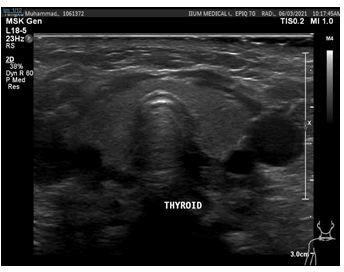
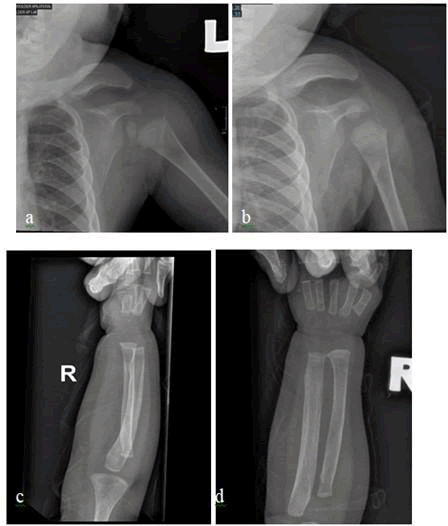
Radiological investigation of left shoulder revealed a cortical discontinuity over midshaft of left clavicle along with surrounding extensive callus formation suggestive of a healing mid clavicle fracture (Image 2a&b). Ultrasonography of left shoulder was also performed to look for any collection due to the overlying swelling and skin changes (Image 3) and it reported cortical irregularity over left clavicle with thickening of subcutaneous tissue over left shoulder is mainly at the anterior and posterior aspects. Child was admitted for continuous observation, and IV Cloxacillin was initiated. Across the days swelling as well as erythematic changes over left shoulder did not resolve. Mantoux test was performed demonstrating a negative result and there was no growth in blood culture test [2-5].
Image 3: Ultrasound of left shoulder demonstrating diffuse subcutaneous oedema with no loculated subcutaneous, or intramuscular collection observed. No effusion seen within the left shoulder joint.
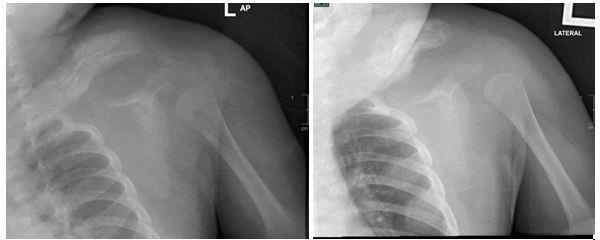
One week later, x-ray of left shoulder was repeated, and comparison was made with previous left shoulder radiograph. There are ill defined lytic changes of the left mid and lateral clavicle observed with extensive long segment periosteal reaction. This is significantly increased compared to the previous radiograph done 1 week ago. There is also marked cortical disruption and cortical thickening suggestive of possible intramedullary extension. However, there were no definite joint disruption seen. Soft tissue swelling is observed adjacent to the left clavicle with preserved fat plane. Overall features of aggressive lytic bone lesion with extensive periosteal reaction (Image 4). MRI was suggested for further evaluation. Infective parameters did not show any improvement hence IV Ceftazidime was added on to cloxacillin [6].
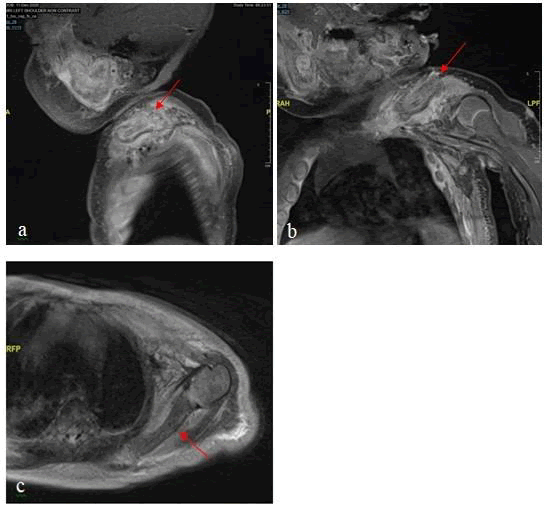
MRI of left shoulder with contrast was done a few days later revealing gross expansion of the left clavicle with diffuse peri-clavicular soft tissue enhancement suggestive of soft tissue inflammatory changes. On the sagittal view, the expanded clavicle can be seen to be made up of multiple concentric rings. The outermost of the concentric ring returns hypointense signal on all sequences - representing the periosteal lining which appears thickened and grossly irregular (Image 5).
Subperiosteal enhancement is observed, likely in keeping with the presence of subperiosteal fluid. Discontinuity of the periosteal lining is observed at both ends of the clavicle, whereby the subperiosteal enhancement is in turn seen in continuity with the surrounding inflammation. A focal break of the periosteal lining is detected at the proximal 1/3 of the clavicle, with no definitive soft tissue collection detected.
The adjacent cortical lining and inner marrow appears generally intact and there is no definite intra-medullary collection detected neither there are sequestrum, involucrum or cloaca. Similar abnormal bony expansion with thickened periosteum and subperiosteal enhancement is also observed diffusely involving the left scapula. Surrounding soft tissue inflammatory changes is also seen at the peri-scapular region however there is no peri-scapular collection [7].
Bony expansion to a lesser degree is also seen involving the adjacent T1 until T7 ribs and subtle enhancement is also seen surrounding the left humeral head, with no overt periosteal thickening or subperiosteal inflammation. There is no shoulder joint effusion. Generalized soft tissue oedema is seen on the anterior chest wall. Overall features are suggestive of osteomyelitis changes involving the left clavicle and scapula; and to a lesser degree T1 to T7 ribs and left humeral head. Surrounding soft tissue inflammation is observed, but no subcutaneous, intra-muscular or intra-articular collection detected [8].
A multidisciplinary team conference was held between General Paediatric Medical Unit, Paediatric Orthopaedic Subspeciality as well as Musculoskeletal Radiology Unit. The diagnosis of multifocal osteomyelitis was established, and additional nuclear imaging investigation Positron Emission Tomography (PET) scan was planned. Rifampicin antibiotic was also added in the combination of drugs to combat the illness.
Throughout stay in ward, child’s oral intake was excellent and there was no documented temperature. On 3rd week of admission, parent also noticed that child’s right forearm developed swelling and redness which was similar to left shoulder symptoms. However clinically left upper limb movement was normal and child was active as usual.
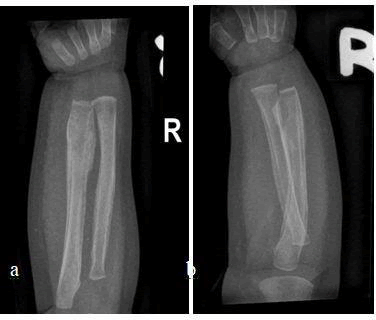
Plain radiograph of right forearm revealed diffuse periosteal reaction throughout radius and ulna bone (Image 6). There was no cortical discontinuity observed. Redness and swelling over right forearm resolved after a few days and patient’s general clinical condition was satisfactory throughout [9-11].
An anterior and posterior whole bone scintigraphy was performed using Technetium-99m MDP. The scan findings are increased radiotracer uptake at temporomandibular area, epiphyseal plates of the humerus, radius, ulna, femur, tibia and fibula which represents the normal growth centres. There is also increase in radiotracer uptake over left clavicle, left scapula, bilateral radius and ulna region in keeping with recent diagnostic finding (Image 7). In view of no significant evidence of collection or foci of infection, there was no role for incision and drainage or biopsy hence antibiotics therapy was continued.
Child completed 8 weeks of IV Cloxacillin, 3 weeks of IV Ceftazidime and 1 week of syrup rifampicin. He was then discharged with another 1-week course of syrup rifampicin to be completed at home. Examination prior to discharge revealed no other obvious swelling nor inflammatory changes over both upper and lower extremity. Active range of movement was satisfactory and child’s general condition clinically improved (Fig.8).
2 weeks later child was reviewed in outpatient clinic, deformity over left shoulder resolved and there were no further swelling observed throughout limbs. Child completed the 2 weeks of rifampicin course, has been active and tolerating orally well at home. There were no episodes of fever. Repeated radiograph of left shoulder and right forearm revealed complete resolution of periosteal reaction and cortical expansion which was previously observed (Image 9).
Infective parameters were also repeated and demonstrated marked improvement compared to baseline taken during initial presentation. Child was given long term follow up to continue observation and reassurance was given to parents who are grateful of the treatment given.
Discussions
Osteomyelitis is an infection of bone and marrow causing progressive destruction and apposition of new bone formation. Infection is usually caused by microorganism and the various routes of transmission are hematogenous, direct inoculation, and local extension from contiguous areas. Acute osteomyelitis commonly occurs in childhood, however the predominant age group at presentation varies between literatures. In children, hematogenous multifocal osteomyelitis is a serious form of osteomyelitis that can swiftly lead to sepsis if it is not addressed in a timely manner. Acute infection foci appear in multiple bones at the same time because of hemorrhagic transmission. Robert et al. in a study on multifocal osteomyelitis in 139 children revealed demographically that 46% were between 6 weeks and 3 years of age (Robert H. et al. 1991).
Clinical presentation
Clinical signs are often nonspecific in the neonatal period in comparison to OM in childhood. Signs described are vague like nutritional difficulties and generalized as well as localized edema, increased tenderness and erythematous skin. Pain sometimes limits movement of the involved extremity. Fever is also non-specific. Thus, clinical presentation can range of severe swelling and inflammatory changes to incidental findings. Penetrating trauma, surgery, invasive procedures (such as umbilical artery catheterization) and prematurity are seen as potential risk factors for hematogenous spread of bacteria.
A study on pathogenesis of OM in children showed that osteomyelitis was situated mainly in the lower limbs, 70% (all lesions) versus 20% for the upper limbs. The lower leg segment was the most frequently involved, amounting to 39.5% of all locations (tibia, 32.3%; fibula 7.2%). The femur and tibia accounted for 58% of all general locations and in upper limb involvement, the humerus was the most frequently affected segment (11.4%) (Labbe´ et al. 2010). Chronic recurrent multifocal osteomyelitis (CRMO) and other perinatal infection should be distinguished from acute haematogenous multifocal osteomyelitis. Symmetrical and bilateral involvement is a known fact in CRMO (Sichardt et al. 2000).
Investigation
As in most of the acute infections, the ESR and CRP levels are found to be elevated in patients. Serial monitoring of these parameters was useful in assessing therapy response and follow-up. A positive blood culture is the strongest sign for developing deep infections like osteomyelitis (OM). In certain cases, antibiotics are started before cultures are obtained, thus a false negative result is conceivable. Blood cultures, on the other hand, are only positive in half of the cases. Diagnostic imaging should be used if there is no distinct focus or a positive blood culture.
In the imaging of paediatric osteomyelitis, a variety of modalities are applicable. Radiographs are commonly obtained, with some investigators maintaining that radiography should always be performed as the first imaging assessment because radiographic findings may exclude other pathologic conditions (Oudjhane K, et.al 2001). Ultrasonography was helpful in soft tissue changes around osteomyelitis as well as confirming the presence of subperiosteal abscess in those children with an appropriate history and localising signs in this study. Sreenivas et.al came across 11 patients (42.3%) in which there were subperiosteal abscess on ultrasonography. This non-invasive modality assists in early diagnosis by visualising the collection for surgical indication.
Computed tomography (CT) provides images with high spatial and contrast resolution and extraordinary cortical bone detail. Nevertheless, the sensitivity of CT for detecting osteomyelitis is generally accepted to be less than the sensitivity values of scintigraphy and magnetic resonance (MR) imaging. Therefore, CT should be reserved for specific diagnostic inquiries and should not be used routinely.
MR imaging has emerged as a valuable tool for targeted investigation when the site of osteomyelitis is clinically evident. MR imaging is indicated in defining the extent of infection and associated soft-tissue abnormalities, including abscesses. Setbacks of MR imaging include the long waiting period due to its availability and high demand as well as increased time of imaging, which necessitates frequent requirements for sedation (Vijayanathan et al 2010).
Scintigraphy is an established tool for evaluating osteomyelitis. Many investigators cite several advantages and advocate the use of scintigraphy as the initial test of choice when radiographically occult osteomyelitis is suspected. Bone radionuclide images are rapidly positive within the first 24–48 hours after the onset of symptoms. Scintigraphy is more useful than MR imaging particularly when the suspected site of osteomyelitis is not clinically evident, such as when the patient has bacteremia, is limping, or refuses to bear weight.
In a scintigraphy protocol, Technetium 99m (99mTc)–labeled diphosphonates localize to areas of active mineralization. A triple-phase bone scintigraphic examination is usually performed, which consists of radionuclide images of the region of interest during an angiographic phase (blood flow phase), a blood pool phase (tissue phase), and a delayed phase. Histological examination of biopsy tissue is important to exclude other diagnoses, such as tumours or histiocytosis however this procedure is only an option if a foci of infection or significant collection detected.
Pathogens
Staphylococcus aureus is a prominent pathogen in neonatal septicemia and carries a high risk of developing deep-seated infections such as OM (Ross et al. 2010). Other commonly found pathogens are Streptococcus agalactiae, Escheria coli, Klebsiella and Enterobacter. Recent studies have pointed that Methicillin Resistant Staphylococcus Aureus (MRSA) has emerged as a major pathogen in acute osteomyelitis (Saavedra-Lozano et.al 2008). The emergence of MRSA in the community has increased the importance of culturing all collections to identify pathogens and to determine antimicrobial susceptibility.
Treatment
Early detection and treatment are critical for a positive outcome. Treatment involves optimal antibiotic regimen, pain management and if necessary, repeated surgical intervention (Korakaki E. et.al 2007). Drainage of abscesses and arthritis should be initiated immediately, after which intravenous treatment should be started as soon as possible. Antibiotic treatment duration for 6-8 weeks is the primary treatment. Antibiotics should correlate with outcome of the bacterial culture [12].
In the presenting case the Staphylococcus aureus was sensible for Cloxacillin, however due to the progression of the infection Ceftadizime and Rifampicin was added. Considering the possible severity of sight effect of Rifampicin, especially in this small premature neonate, we limited the duration of treatment to 2-weeks compared to Ceftazidime(3-weeks) and Cloxacillin(8-weeks) which was given on prolong duration.
Sequential parenteral-oral therapy may be used with close follow up. Shorter duration of parenteral therapy followed by oral therapy based on good clinical response was not associated with recurrence of infection. If the clinical response to therapy is satisfactory, antibiotics can be continued orally (Peltola H et.al 2009). However no specific evidence-based recommendations can be made, and no specific time markers are described in the literature (Caramia G et.al 2007). Peltola et al proposed a shorter treatment in patients older than 3 months.
McPherson et al. revealed in a study that duration of parenteral therapy followed by oral therapy based on good clinical response was not associated with recurrence of infection. Since few reports of OM in new-borns have been published no specific guidelines are available for premature babies suffering from multifocal osteomyelitis. In the presenting case we continued the antibiotics for a prolong duration while analysing patients clinical and infective parameters. Surgical incision and drainage may be performed in the presence of abscesses and collection surrounding region of osteomyelitis.
Deshpande et al., reviewed 15 cases of neonatal septic arthritis and advised immediate arthrotomy to drain pus from the joint in case of strong clinical suspicion, instead of waiting 72 h. This resulted in a better long-term outcome with less functional sequelae. Long term outpatient follow up after discharge is vital especially newborns with multifocal osteomyelitis as any evidence of relapse may be identified early and managed. Better long-term results can be achieved by early surgical drainage and immediate appropriate antibiotic coverage [13,15].
Conclusion
Although all identified cases were caused by Gram-positive organisms, the empiric initial treatment should also cover Gram-negative organisms because of their well-known involvement in neonatal osteomyelitis. The diagnosis of paediatric osteomyelitis is often clinically difficult. Nevertheless, a paediatric osteomyelitis diagnosis can be confidently made with scintigraphy when the radiograph is normal. Compared with other modalities, bone scintigraphy is particularly useful when the site of osteomyelitis is unclear. The response to antibiotics in this patient was moderate and her symptoms settled completely ten months after their onset and have not recurred. In one case repeated flare-ups of symptoms from a proximal. It is important to emphasize the fact that adequate and timely surgical intervention, along with antibiotics, is essential in the management of acute haematogenous multifocal osteomyelitis to minimise morbidity we advocate clinical observation and infective parameters as a guide in duration of parenteralantibiotics.
References
- Arnold SR, Elias D, Buckingham SC, et al. Changing patterns of acute hematogenous osteomyelitis and septic arthritis: emergence of community-associated methicillin-resistant Staphylococcus aureus. J Pediatr Orthop 2006;26(6):703–708.
- Borzutzky A. Stern S. Reiff A. et al. Pediatric chronic nonbacterial osteomyelitis. Pediatrics. 2012; 130: e1190-e1197
- Caramia G, Ruffini E, Zaffanaello M, Fanos V Acute bone and joint infections inchildren and therapeutic options. J Pediatr Infect Dis 2: 193-203(2007).
- Deshpande SS, Taral N, Modi N, Singrakhia M Changing epidemiology of neonatal septic arthritis. J Orthop Surg (Hong Kong) 12: 10-1 (2004).
- Fritz J. The contributions of whole-body magnetic resonance imaging for the diagnosis and management of chronic recurrent multifocal osteomyelitis. J Rheumatol. 2015;42(8):1359–60
- Guérin-Pfyffer S, Guillaume-Czitrom S, Tammam S, Koné-Paut I. Evaluation of chronic recurrent multifocal osteitis in children by whole-body magnetic resonance imaging. Joint Bone Spine. 2012;79(6):616–20.
- Hermann Girschick, Martina Finetti, Francesca Orlando, , Marco Gattorno, Paediatric Rheumatology International Trials Organisation (PRINTO) and the Euro fever registry, The multifaceted presentation of chronic recurrent multifocal osteomyelitis: a series of 486 cases from the Euro fever international registry, Rheumatology, Volume 57, Issue 7, July 2018
- Hofmann, S.R., Kapplusch, F., Girschick, H.J. et al. Chronic Recurrent Multifocal Osteomyelitis (CRMO): Presentation, Pathogenesis, and Treatment. Curr Osteoporos Rep 15, 542–554 (2017).
- Jansson A.F. Grote V. Nonbacterial osteitis in children: data of a German Incidence Surveillance Study. Acta Paediatr. 2011; 100: 1150-1157
- Korakaki E, Aligizakis A, Manoura A, Hatzidaki E, Saitakis E, et al. (2007) Methicillin-resistant Staphylococcus aureus osteomyelitis and septic arthritis in neonates: diagnosis and management. Jpn J Infect Dis 60: 129-131.
- Labbe´ JL, Peres O, Leclair O et al (2010) Acute osteomyelitis in children: the pathogenesis revisited? Orthop Traumatol Surg Res 96(3):268–275
- Marion R Roderick, Ethan S Sen, Athimalaipet V Ramanan, Chronic recurrent multifocal osteomyelitis in children and adults: current understanding and areas for development, Rheumatology, Volume 57, Issue 1, January 2018, Pages 41–48,
- Mellado Santos JM. Diagnostic imaging of pediatric hematogenous osteomyelitis: lessons learned from a multi-modality approach. Eur Radiol 2006;16(9): 2109–2119.
- Oliver M. Lee T. Halpern-Felsher B. et al. Disease burden and social impact of chronic nonbacterial osteomyelitis on affected children and young adults. Arthriti Rheumatol. 2017; 69
- Oudjhane K, Azouz EM. Imaging of osteomyelitis in children. Radiol Clin North Am 2001;39(2): 251–266
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences