Passive Pronosupination is not Valuable in Prediction of Radius Malreduction
Shields DW, Marsh MA, Aldridge SE and Williams JR
DOI10.4172/2471-8416.100019
Shields DW*, Marsh MA, Aldridge SE and Williams JR
Department of Trauma and Orthopaedics, Royal Victoria Infirmary, Queen Victoria Road, Newcastle-Upon-Tyne, NE1 4LP, UK
- *Corresponding Author:
- David William Shields
Department of Trauma and Orthopaedics
Royal Victoria Infirmary
Queen Victoria Road
Newcastle-Upon-Tyne
NE1 4LP, UK
E-mail: dwshields@gmail.com
Received date: March 07, 2016; Accepted date: May 26, 2016; Published date: May 30, 2016
Citation: Shields DW, Marsh MA, Aldridge SE, Williams JR (2016) Passive Pronosupination is not Valuable in Prediction of Radius Malreduction. J Clin Exp Orthop 2:19. doi: 10.4172/2471-8416.100019
Copyright: © 2016 Shields DW, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The management of displaced diaphyseal forearm fractures in adults is predominately operative. Anatomical reduction is necessary to infer optimal motion and strength. The authors have observed an intraoperative technique where passive pronosupination is examined to assess quality of reduction as a surrogate marker for active movement.
We aimed to assess the value of this technique by intentionally malreducing a simulated diaphyseal fracture of a radius in a cadaveric model, and measuring the effect on pronosupination.
A single cadaveric arm was prepared and pronation supination was examined according to American Academy of Orthopaedic Surgeons guidance. A volar "Henry" approach was then performed and a transverse osteotomy achieved in the radial diaphysis. A locking plate was used to hold the radius in progressive amounts of translation and rotation, with changes in pronosupaintion measured with a goniometer.
The radius could be grossly malreduced with no effect on pronation and supination until the extremes of deformity. The forearm showed more tolerance with rotational malreduction than translation. Passive pronation was more sensitive for malreduction than supination.
The use of passive pronosupination to assess intraoperative quality of reduction is misleading and not advised.
Keywords
Forearm; Fracture; Cadaver; Fixation; Function; Motion
Introduction
Teaching from the AO group states that, when managing forearm fractures anatomical reduction is essential and as such the forearm should be treated as a joint [1-3]. In contrast to closed reduction and cast immobilisation which has been shown to have poor results [4], accurate reduction has been verified to improve range of motion [4-9]. Even with anatomical reduction however, a decline in function, strength and range of motion is to be expected [5-7], with results better in the long term in patient who were skeletally immature at the time of injury [8]. Thus where possible, accurate reduction and absolute stability should be employed in order to optimise forearm function [9], with no detectable difference between locked compression plates (LCP) and limited contact dynamic compression plates (LC-DCP) [10-12]. The subcutaneous nature of the ulna lends itself to ease of exposure and accurate reduction which, combined with it’s straight osteology, infrequently results in malreduction. In contrast, even with an open approach to the radius it can difficult to visually inspect the full extent of the reduction, particularly with more proximal fractures where muscle bulk can impede vision. In order to fully expose the entire fracture site particularly with the radius, would require excessive soft tissue stripping. Frequently the surgeon encounters comminution, and judging the correct length, alignment and rotation can be difficult.
A technique which the authors have seen employed to assess quality of reduction (in particular comminuted fractures), is to passively examine the range of pronation and supination. The aim of the technique is to evaluate any ‘mechanical’ block’ which would in turn limit function. The criticism of this method is that passive movement is not necessarily representative of active movement, and should not be used as a surrogate marker of fracture reduction.
There is good evidence so show the effect of malreduction of active forearm movement, however there is no evidence directly examining the effect of malreduction on passive movement to verify this ‘mechanical block’ test.
Aims
We wished to investigate the value of this testing passive pronosupination in a malreduced radius in both rotation and translation.
Hypothesis
The forearm would poorly tolerate malreduction resulting in a reduction in passive pronosupination.
Method
A single fresh frozen cadaver arm was prepared and ‘baseline’ pronation and supination was measured using American Academy of Orthopaedic Surgeons guidance [13].
This baseline was in keeping with the range of motion in clinical practice confirming its validity of use in this study. A Henry approach to the radial diaphysis was performed and transverse osteotomy in the middle of the diaphysis was achieved with osteotomes. No further soft tissue stripping was undertaken. A transverse osteotomy was used to allow pure rotation and translation without unintended shortening/ lengthening at the osteotomy site.
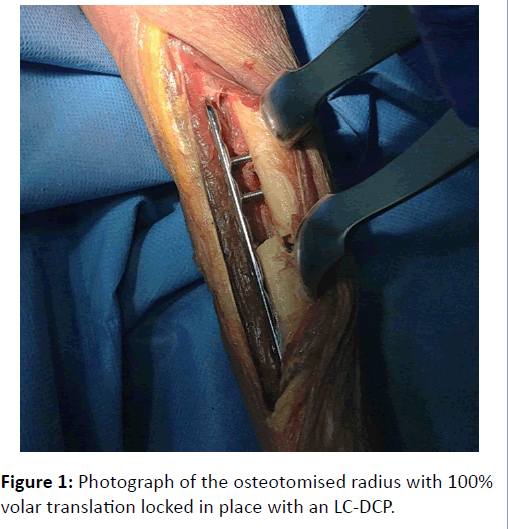
An 8 hole locking plate (Synthes, Solothurn, Switzerland) was applied on the volar surface of the radius bridging the osteotomy, and held in place with locking screws (Figure 1). 2 parallel k-wires were introduced, one on each side of the osteotomy, and used as a reference point for rotation. The locking plate was used to minimise chance of plate loosening/ failure during the experiment. The proximal radius was then sequentially malreduced rotationally in 10 degree increments both directions, with the plate being locked for each measurement. For each increment, pronation and supination was measured using a goniometer and recorded by two observers, until a ‘block’ to rotation occurred.
For malreduction in the volar/dorsal plane, we measured proportions of the radius diameter (50%, 100% in a volar and dorsal direction). At each proportion of malreduction, the plate was ‘locked’ and pronation/supination was measured and agreed by 2 observers. The same method was used in an ulnar/radial direction. More than 2 measurements would have required additional screw holes, running the risk of comminuting the radius.
Ethics
Ethical considerations fell under local cadaveric laboratory approval.
Results
Initial examination of the forearm revealed pronation of 80 degrees and supination of 90 degrees.
Rotation: As shown in Table 1, limitation of passive movement was not limited until the distal fragment was externally rotated by 45 degrees, or internally rotated to 40 degrees.
| Rotation (degrees) | Pronation (degrees) | Supination (degrees) |
|---|---|---|
| Anatomical | 80 | 90 |
| Externally 25 | 80 | 90 |
| Externally 30 | 80 | 90 |
| Externally 35 | 80 | 90 |
| Externally 40 | 80 | 90 |
| Externally 45 | 60 | 90 |
| Internally 25 | 80 | 90 |
| Internally 30 | 80 | 90 |
| Internally 35 | 80 | 90 |
| Internally 40 | 70 | 90 |
Table 1: Range of movement of the osteotomised radius with progressive rotation of the distal fragment
Translation: As shown in Table 2, limitation of pronation and supination did not occur until the radius was displaced 100% in an ulnar direction or radial direction. Limitation did occur at 50% displacement in volar and dorsal directions. Interestingly, supination was only affected by maximal (i.e. 100%) displacement in a radial direction, which is in contrast to previously thought [14].
| Translation | Pronation (degrees) | Supination (degrees) |
|---|---|---|
| Anatomical | 80 | 90 |
| Ulnar 50% | 80 | 90 |
| Ulnar 100% | 46 | 90 |
| Radial 50% | 80 | 90 |
| Radial 100% | 32 | 80 |
| Volar 50% | 63 | 90 |
| Volar 100% | 40 | 90 |
| Dorsal 50% | 54 | 90 |
| Dorsal 100% | 23 | 90 |
Table 2: Range of movement of the osteotomised radius with progressive translation of the distal fragment.
The investigators noted that towards extremes of external rotation (beyond 30 degrees) that the interosseous membrane became tight; however, this did not necessarily limit range of movement.
Limitations
This study is only a single cadaveric study, due to limitation of resources, so does not allow for a wide variety of anatomical variations. We were unable to test concomitant malreduction of the ulna without additional soft tissue dissection, which would devalue the results we have found. The quality of bone stock prevented evaluation of further types of malreduction (i.e. shortening and angulation) however these are more researched within published literature of having low tolerance for malreduction, therefore testing passive motion in these circumstances are even less likely to give falsely normal ranges.
Whilst rotation broadly occurs in the axis of the ulna which is static with the radius rotating around the ulna it could be argued that malreduction of the ulna is a more important clinical pitfall. Our clinical experience is that due to the subcutaneous nature of the ulna achieving accurate reduction is more difficult in the radius, thus we focussed this study on radial malreduction.
Conclusion
The aim of operative intervention in forearm trauma is to maximise functional outcome, i.e. strength and active motion. In order to achieve this, it has been shown within the literature the requirement of anatomical reduction. We discovered that we could intentionally malreduce the radius, with no effect on range of passive movement. Therefore, an examination of passive movement intraoperatively will not predict ultimate active range of movement.
Malrotation of the radius was seen to cause restriction on the soft tissues by pulling the interosseous membrane taught, however passive pronosupination was not effected. It could be this tense membrane which limits active range of movement, which would not be detected passively.
The use of passive tests to evaluate the reduction in both rotation and AP translation can be misleading. Our results indicate the use of passive pronation and supination is ineffective and does not add value to the assessment of intraoperative radius reduction.
Authors Contributions
This study was conceived and designed amongst all the authors. The study was carried out by DWS and data verified by MAM. Analysis and drafting of the manuscript received contributions from all authors.
Acknowledgements
The authors would like to acknowledge the Newcastle Surgical Training Centre for the use of their facilities for this study.
References
- Ruedi T, Buckley R (2007) AO Principles of Fracture Management, Books and DVD. Thieme.
- Muller ME, Allgöwer M, Willenegger H (1965) Technique of Internal Fixation of Fractures. New-York.
- Jayakumar P, Jupiter JB (2014) Reconstruction of maluniteddiaphyseal fractures of the forearm. HAND. SAGE Publications 9:265–273.
- Jupiter JB, Fernandez DL, Levin LS, Wysocki RW (2009) Reconstruction of Posttraumatic Disorders of the Forearm. J Bone Joint Surg Am. The American Orthopedic Association91:2730–2739.
- Goldfarb CA, Ricci WM, Tull F, Ray D, Borrelli J (2005) Functional outcome after fracture of both bones of the forearm. Journal of Bone & Joint Surgery, British Volume87:374–379.
- Droll KP, Perna P, Potter J, Harniman E, Schemitsch EH, et al. (2007) Outcomes following plate fixation of fractures of both bones of the forearm in adults. The Journal of Bone & Joint Surgery89:2619–2624.
- Schulte LM, Meals CG, Neviaser RJ (2014) Management of adult diaphyseal both-bone forearm fractures. J Am AcadOrthopSurg22:437–446.
- Bot AGJ (2011) Long-Term Outcomes of Fractures of Both Bones of the Forearm. J Bone Joint Surg Am 93:527–526.
- Iacobellis C, Biz C (2014) Plating in diaphyseal fractures of the forearm. Acta Bio MedicaAteneiParmensis.
- Saikia KC, Bhuyan SK, Bhattacharya TD (2011) Internal fixation of fractures of both bones forearm: Comparison of locked compression and limited contact dynamic compression plate. Indian journal.
- Richard MJ, Ruch DS, Aldridge JM III (2007)Malunions and Nonunions of the Forearm. Hand Clinics23:235–243.
- Nasab S, Sarrafan N, Arti H (2012) Outcome of forearm shaft fractures in adults treated by open reduction and internal fixation with Dynamic Compression Plate (DCP). Pak J Med Sci.
- American AOOS (1965) Joint Motion: Method of Measuring and Recording. Amaerican Academy of Orthopaedic Surgeons.
- Dumont CE, Thalmann R, Macy JC (2002) The effect of rotational malunion of the radius and the ulna on supination and pronation. Journal of Bone & Joint Surgery, British Volume84:1070–1074
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences