Quantative Analysis of Glenoid Labral Volume Using MRI
Anoop Krishna*, Shyam Sundar and Jonathan Negu
Department of Orthopedics, Ortho One Orthopaedic Speciality Centre, Coimbatore, Tamilnadu, India
- *Corresponding Author:
- Anoop Krishna
Department of Orthopedics,
Ortho one Orthopaedic Speciality Centre, Coimbatore, Tamilnadu,
India,
E-mail: dranoopkrishna@icloud.com
Received date: March 01, 2023, Manuscript No. IPJCEOP-23-6004; Editor assigned date: March 03, 2023, PreQC No. IPJCEOP-23-6004(PQ); Reviewed date: March 14, 2023, QC No. IPJCEOP-23-6004; Revised date: March 24, 2023, Manuscript No. IPJCEOP-23-6004 (R); Published date: March 31, 2023, DOI: 10.36648/2471-8416.9.3.105
Citation: Krishna A, Sundar S, Negu J (2023) Quantitative Analysis of Glenoid Labral Volume using MRI. J Clin Exp Orthopr Vol.9 No.3:105
Abstract
The glenoid labrum is a fibrocartilage in the shoulder joint, anchoring the joint capsule and shoulder ligaments. It helps in improving the joint congruity and increases the contact surface area. Morphology varies regionally, especially in the superior and anterior region; these variants can sometimes be confused with pathological conditions. The labrum is often involved in shoulder instability, by single macro trauma or, more often, repetitive microtrauma. It is triangular in cross section with its base fixed to the edges of the glenoid while the free edge is thin and sharp.
Keywords
Repetitive microtrauma; Glenoid; Morphology; Labrum; Labroligamentous
Introduction
In patients with recurrent anterior instability of shoulder, anterior glenoid surface and labrum are often damaged. The degree and type of damage varies in patients. A detailed quantitative analysis of bony glenoid shape has been reported using MRI and 3D CT, however a quantitative analysis of la-brum has not been reported. Our hypothesis was that in patients with recurrent shoulder instability, the quality of the labrum is inferior to the normal. Assessing the labral morphology using MRI would help us prepare for intraoperative management of defective labrum and helps us in anticipating the prognosis. We also put forth a classification for the torn labrum. The aim of the study was to quantitatively assess the volume of labrum in normal population and to compare it with those patients with recurrent shoulder instability. We have also classified it according to the volume of the labrum [1].
Aim
The aim of the study was to quantitatively assess the volume of labrum in normal population and to compare it with those patients with recurrent shoulder instability.
Methodology
This was a retrospective MRI based double blinded observational study conducted between January 2014 to December 2015 [2].
Among the 130 patients who underwent MRI from 2014 to 2015, 34 patients with normal labrum (diagnosed by an experienced radiologist) were taken as control.
Skeletally mature individuals, samples with age less than 50 years with history recurrent shoulder instability were included in this study. Patients over the age of 50 years with age related changes in labral volume, patients with associated shoulder lesions (fractures involving glenoid, humeral head, cystic lesions in the shoulder joint) were excluded. Out of this sample group 50 patients had labral injury [3].
All the MRI s (GE Signa Excite 1.5 T) was taken with position of the shoulder joint at 0 degrees of flexion and abduction with neutral rotation [4].
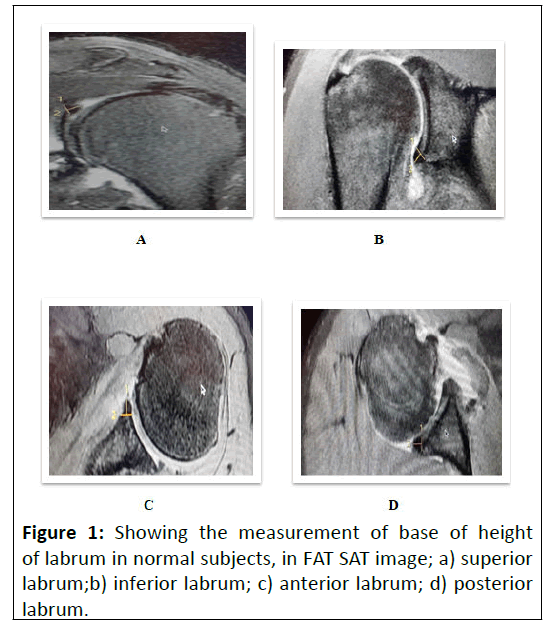
Measurements were made in Axial fat sat and Coronal T2 fat sat sections which clearly depicts the labral dimensions. Superior labrum was measured in the plane where the long head of biceps looked smallest and labrum was largest, usually at the 12 ’O position.
Anterior and posterior labrum was measured in the axial sections at the level of insertion of the anterior inferior glenoid ligament. Uninjured labral measurements (base, height) were made in 30 patients, who fell into the inclusion criteria, to find out the normal dimensions [5].
Measurements of the injured labrum were measured and compared with the initial readings to find out difference in dimensions ( Figure 1).
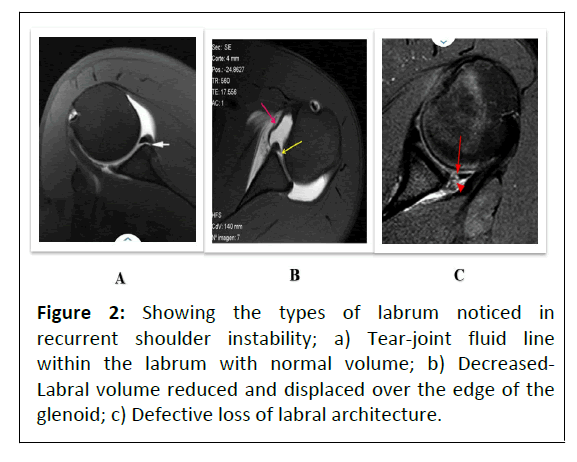
Measurements of the injured labrum were measured and compared with the initial readings to find out difference in dimensions [6,7]. Shape of the injured anterior labrum was compared with the normal labrum and were classified into three types (Figure 2).
Shape of the injured anterior labrum was compared with the normal labrum and were classified into three types [8].
Torn: Volume of the labrum remained normal, but the white line (joint fluid line) which indicates a tear in the labrum architecture.
Decreased: Volume is decreased, but anterior labrum remained on the edge of the glenoid.
Defective: Anterior labrum was not visualised on the anterior edge of the glenoid
Two orthopaedic specialists and one radiologist measured the labral morpholo-gy as per the guidelines. Inter observer and Intraobserver reliability were analysed using ICC [9].
Results
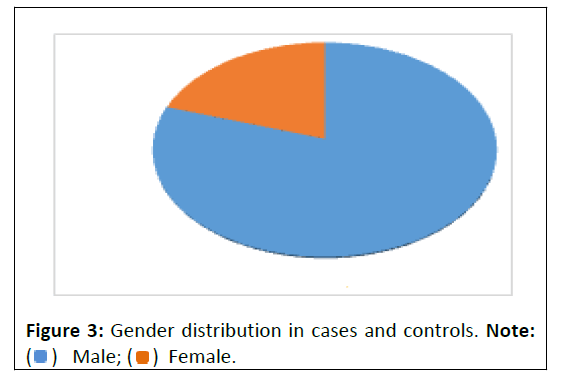
Total of 130 shoulders were initially studied considering the exclusion criteria. MRIs of 84 subjects were observed and measurements recorded for this study. The subjects were aged 29.8 ± 5.1 ranging from 20 to 47 years. MRIs studied were of subjects that were predominantly (91.7%) male (Figure 3).
Of them 34 (40.5%) were MRIs of subjects who did not have any labral pathology, while the rest (n=50) had labral lesion.
All measurements were made by three observers. Inter observer and intra observer reliability was 0.86 and 0.88 respectively as per ICC which was excel-lent. In normal subjects (Table 1) the average measurements were -7.8 mm (Base) and 5.2 mm (Height) for superior labrum, 6.5 mm (base) and 5.5 mm (height) for inferior labrum, 5.4 mm (Base) and 5.9 mm (height) for anterior labrum, 4.8 mm (Base) and 4.9 mm (height) for posterior labrum [10]. Measurements for patients with labral tear (Table 2 ) was found to be 7.74 mm (base) and 5.29 mm (height) for superior labrum, 6.43 mm (Base) and 5.51 mm (height) for inferior labrum, 4.7 mm (base) and 5.3 mm (height) for anterior labrum, 4.6 mm (base) and 4.76 mm (height) for posterior labrum (Tables 1 and 2).
| Superior labrum |
Inferior labrum |
Anterior labrum |
Posterior labrum |
|||||
|---|---|---|---|---|---|---|---|---|
| Base | Height | Base | Height | Base | Height | Base | Height | |
| Observer1 | 7.8 | 5.2 | 6.5 | 5.5 | 5.4 | 5.9 | 4.8 | 4.9 |
| Observer 2 | 7.72 | 5.21 | 6.6 | 5.54 | 5.4 | 5.85 | 4.86 | 4.9 |
| Observer 3 | 7.76 | 5.19 | 6.5 | 5.51 | 5.4 | 5.91 | 4.8 | 4.92 |
Table 1: Dimensions in normal glenoid labrum (control).
| Superior labrum |
Inferior labrum |
Anterior labrum |
Posterior labrum |
|||
|---|---|---|---|---|---|---|
| Base | Base | Height | Height | Base | Height | |
| Observer 1 | 7.74 | 6.43 | 5.51 | 5.31 | 4.6 | 4.76 |
| Observer 2 | 7.7 | 6.6 | 5.6 | 5.34 | 4.62 | 4.74 |
| Observer 3 | 7.68 | 6.4 | 5.5 | 5.32 | 4.64 | 4.7 |
Table 2: Dimensions of labrum in subjects with instability.
Labral tears were classified according to the volume of the anterior labrum [11]. Base and height was found to be decreasing with the degree of tear with type 3 showing maximum reduction in dimensions (Table 3 ). Posterior labral dimension was found to effect on in those with Type 3 labral injury (Tables 3 and 4).
| Classification | Samples | Observer 1 | Observer 2 | Observer 3 | |
|---|---|---|---|---|---|
| Type 1 | 13 | 5.66 | 5.18 | 5.2 | 5.61 |
| Type 2 | 19 | 5.32 | 4.76 | 4.8 | 5.3 |
| Type 3 | 18 | 5.08 | 4.2 | 4.2 | 5.1 |
Table 3: Dimensions of anterior labrum in patients with instability.
| Classification | Sample | Observer 1 | Observer 2 | Observer 3 | |
|---|---|---|---|---|---|
| Height | Base | Base | Height | ||
| Type 1 | 13 | 4.9 | 4.84 | 4.8 | 4.9 |
| Type 2 | 19 | 4.94 | 4.81 | 4.8 | 4.89 |
| Type 3 | 18 | 4.4 | 4.1 | 4.1 | 4.4 |
Table 4: Dimensions of posterior labrum in patients with instability.
The mean superior Labrum height (p-0.175) as well as Inferior labrum’s base (p-0.125) and height (p-0.420) were not statistically significantly different between normal and shoulders with labral lesion [12]. Whereas, rest of the measurements showed statistically significant difference (p<0.05).
These results imply that all measurements (except Inferior labrum and superior labrum height) from MRIs were distinctly different and could be used for screening stable and unstable shoulders. The variables such as age and gender did not show statistically significant difference between the normal and labral tear group (p-0.185 and 1.0, respectively) implying that the MRIs were comparable [13].
Based on our criteria the MRIs with labral lesion were classified into Type I, II and III. Accordingly, 13 (26.0%) could be labeled as Type I, 19 (38.0%) as Type II and 18 (36.0%) as Type III.
Principal component analysis revealed that the anterior and posterior labrum measurements (base and height) were loaded in the one factor, while the inferior labrum base and inferior labrum height were loaded in separate factors. It is clear that the anterior labrum and posterior labrum measurements are highly correlated with each other, while being different from the rest of the measurements [14].
A Multiple Logistic Regression with categorization by observation (normal/labral lesion) as the dependent variable and the labrum measurements as independent variables was performed in order to pick out the variables that significantly distinguished between the two groups, in presence of other variables.
All the labrum variables were included into the model using Enter method. The result revealed that anterior labral base and posterior labral height showed statistically significant difference between stable and unstable shoulders in presence of other labrum measurements (Table 5).
| Labrum | B |
|---|---|
| Inferior Base | 2.6 |
| Inferior height | -3.2 |
| Anterior base | -14.4 |
| Anterior height | -8.5 |
| Posterior base | -2.3 |
| Posterior height | 8.9 |
Table 5: MLR of labrum measurement with stability of shoulder as dependent variable.
Analysis of variance results comparing mean labrum measurement variables between the three classifications made based on observation of MRIs of shoulders with labral lesions are presented in Table 6.
| Labrum | Type | SD | p value |
|---|---|---|---|
| Superior base | I | 0.2 | 0.685 |
| II | 0.2 | ||
| III | 0.3 | ||
| Superior height | I | 0.2 | 0.206 |
| II | 0.2 | ||
| III | 0.3 | ||
| Inferior base | I | 0.4 | 0.348 |
| II | 0.2 | ||
| III | 0.2 | ||
| Inferior height | I | 0.3 | 0.08 |
| II | 0.2 | ||
| III | 0.2 | ||
| Anterior base | I | 0.1 | <0.0001 |
| II | 0.1 | ||
| III | 0.1 | ||
| Anterior height | I | 0.1 | <0.0001 |
| II | 0.1 | ||
| III | 0.1 | ||
| Posterior base | I | 0.1 | <0.0001 |
| II | 0.1 | ||
| III | 0.1 | ||
| Posterior height | I | 0.2 | <0.0001 |
| II | 0.1 | ||
| III | 0.3 |
Table 6: Comparison of mean labrum measurements between types.
Superior and inferior labrum measurements (both base and height) did not show and stastically significant difference between the three types (p>0.05) (Table 6). Anterior and Posterior labrum (both base and height) showed a statistically significant difference in the mean values (p<0.05) [15].
Figures are presented as number and percentages. Descriptive statistics is ex-pressed as mean ± 1SD. Independent t test was employed to compare mean values of glenoid volume variables between labral tear group and control group. Analysis of Variance (ANOVA) was employed to compare the same between the three classifications. A Principal Component Analysis (PCA) was conducted to explore and understand the underlying relationships between the measurement variables. Multivariate logistic regression was used to identify variables that significantly contributed in distinguishing between bankarts lesions and control groups. A Receiver Operating Characteristic (ROC) curve was drawn and Area Under the Curve (AUC) was calculated to identify optimal cut off values for usage of variables for screening and their viability.
Discussion
The recurrence rate after primary anterior shoulder dislocation has been repored to be between 17% and 100%. Generally, the Bankart lesion has been thought to be the most common lesion associated with anterior shoulder joint dislocation. Causes of glenohumeral instability vary from traumatic capsule labral disrutions to more severe lesions that include loss of glenoid bone. Bankart lesions occur in over 90% of cases and are characterized by detachment of the labrum from the anteroinferior glenoid. Various forms of anterior inferior labral lesions were seen in patients with traumatic anterior dislocation of shoulder. The recurrent dislocation group showed a significantly higher prevalence of anteroinferior lbral lesions and bony lesions in com- parison with the primary group. Recurent anterior shoulder instability has also been associated with severe Anterior Labroligamentous Periosteal Sleeve Avulsion (ALPSA) lesions. This is first of its kind study to quantitatively assess the volume of glenoid labrum. An intact anteroinferior glenolabral complex not only provides restraint to anterior hmeral translation in the abducted and externally rotated position, but also deepens the glenoid and provides a bumper effect to the anterior glenoid margin. Negative intraarticular pressure in the setting of an intact capsule also creates a stabilizing suction effect. Anteroinferior dislocation is the most frequent cause of anterior glenohumeral instability and produces a constellation of lesions (anteroinferior labral tear, classic and osseous Bankart lesions, Hill-Sachs lesion). Bankarts lesion, which is considered as the essential pathognomonic lesion occurs in 97% of first time acute traumatic dislocations in young patients. Soft tissue bankarts lesion represent complete avulsion of anteroinferior glenolabral complex (the anteroinferior labrum and anterior band of IGHL) from the scapula and rupture of scapular periosteum. Because of its essential stabilising functions, the lbrum must be anatomically restored in patients with instability [16].
The labroligamentous complex will be displaced medially in many patients. In some patients, labrum is displaced medially and rolls up on itself like a sleeve. The labrum then heals in this abnormal medialised position (ALPSA). In such cases the labroligamentous complex should be mobilised surgically and released from the underlying subscapularis so that it can be reattached at its correct atomical location.
MR arthrographic variability of the arthroscopically normal glenoid labrum both qualitatively and quantitatively. In the study there was no significant relationship between quantitative dimensions and arthroscopically normal or abnormal status of the labrum. Quantitatively asses the superior labrum has measured the superior labrual dimensions, 8.5 (Base), 4.9 (height). Our study shows that the volume of labrum decreases in those with recurrent shoulder instability. In Type 1 (torn) the labrum might be injured at the anterior edge of the glenoid. The amount of retained labrum was found to have a significant loss of volume (both height and base) and it does not widen the width of the glenoid surface to prevent a further dislocation. In type 2 and 3 (decreased and defective) labrum was outside the rim of the glenoid. With the increased displacement of the labrum, from type 1 to type 3, the difficulty in mobilising the labrum back to anatomical position increases.
The limitations of this study were that it was a retrospective observational study and hence the clinical outcome measures following repair of defective labrum was not analysed. The MRI features of poor quality labrum was not correlated arthroscopically which would have further guided in optimising the treatment for instability.
Conclusion
Anterior labral base and height were the two measurements that clearly distinguished between bankarts lesion and control group that were classified based on our guideline. Anterior measurements were different between the types I, II and III among the bankarts lesions group. The classification was expressed by smaller tapering glenoid volume in our study. However, these measurements may not be useful for screening purposes (AUC<0.5).
The width and the height of the anterior labrum decreases in patients with labral injury. Classification of the tears according to the volume of the labrum gives us an idea about the extent of damage in the labrum, according to which the surgical treatment can be planned. Labral volume was found to be decreased with increase in the degree of tear.
References
- Clavert P (2015) Glenoid labrum pathology. Orthop Traumatol: Surg Res 101: S19-S24.
- Huijsmans PE, Haen PS, Kidd M, Dhert WJ, van der Hulst VP, et al. (2007) Quantification of a glenoid defect with three-dimensional computed tomography and magnetic resonance imaging: A cadaveric study. J Shoulder Elb Surg 16: 803-809.
- Habermeyer P, Schuller U, Wiedemann E (1992) The intra-articular pressure of the shoulder: An experimental study on the role of the glenoid labrum in stabilizing the joint. Arthrosc J Arthrosc Relat. Surg 8: 166-172.
- Im TS, Choi JA, Oh JH (2014) Superior labral dimension of the glenohumeral joint on direct MR Arthrography (MRA): Relationship with presence of SLAP (Superior Labrum Anterior to Posterior) lesion. J Korean Soc Magn Reson Med 18: 193-199.
- Beltran J, Rosenberg ZS, Chandnani VP, Cuomo F, Beltran S, et al. (1997) Glenohumeral instability: Evaluation with MR arthrography . Radiographics 17: 657-673.
- Taylor DC, Arciero RA (1997) Pathologic changes associated with shoulder dislocations: arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. Am J Sports Med 25: 306-311.
[Crossref] [Google Scholar]Zanetti M, Carstensen T, Weishaupt D, Jost B, Hodler J (2001) MR arthrographic variability of the arthroscopically normal glenoid labrum: qualitative and quantitative assessment. Eur Radiol 11: 559-566. [Crossref] [Google Scholar]
- Aston Jr Jw, Gregory CF (1973) Dislocation of the shoulder with significant fracture of the glenoid. J Bone Joint Surg Am 55: 1531-1533.
- McLaughlin HL (1960) Recurrent anterior dislocation of the shoulder: I. Morbid anatomy. Am J Surg 99: 628-632.
- Neviaser TJ (1993) The anterior labroligamentous periosteal sleeve avulsion lesion: A cause of anterior instability of the shoulder. Arthrosc J Arthrosc Relat Surg 9: 17-21.
- Cooper DE, Arnoczky SP, O'brien SJ, Warren RF, Dicarlo E, et al. (1992) Anatomy, histology, and vascularity of the glenoid labrum. An anatomical study. J Bone Jt Surg 74: 46-52.
- Rowe CR, Patel D, Southmayd WW (1978) The Bankart procedure: A long-term end-result study. J Bone Jt Surg 60: 1-16.
- Taylor DC, Arciero RA (1997) Pathologic changes associated with shoulder dislocations: Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. Am J Sports Med 25: 306-311.
- Baker CL, Uribe JW, Whitman C (1990) Arthroscopic evaluation of acute initial anterior shoulder dislocations. Am J Sports Med 18: 25-28.
- Spatschil A, Landsiedl F, Anderl W, Imhoff A, Seiler H, et al. (2006) Posttraumatic anterior-inferior instability of the shoulder: Arthroscopic findings and clinical correlations. Arch Orthop Trauma Surg 126: 217-222.
- Kim DS, Yoon YS, Yi CH (2010) Prevalence comparison of accompanying lesions between primary and recurrent anterior dislocation in the shoulder. Am J Sports Med 38: 2071-2076.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences