Abstract
Traumatic brain injury result in accelerated fracture healing: A Rat Model
Background: In patients who have sustained a traumatic brain injury with an associated extremity fracture there is often a clinical perception that the rate of new bone formation around the fracture site is increased. In this study, we made a rat model of femoral fracture to investigate the serum factors changes in vivo. We examined the effects serum factors on fracture healing and the molecular signaling pathways that might link these two. Methods and Findings: Thirty-Six female Sprague-Dawley rats were randomly allocated into 4 groups; the non-operated control group, traumatic brain injury (TBI) group, bone fracture (Fr) group and the bone fracture/ TBI group (TBI & Fr) (n=9 per group). These animals were sacrificed at 6 weeks after experiments. Volume of callus in fracture was measured weekly with the Perkins volume formula at 2nd week after operation. The radiology imaging was interpreted by two or more senior orthopedic specialists. In vivo chemo taxis assay by serum samples collected at the 1, 3, 7 and 14 days, and 3rd, 4th, 6th week after surgery. Seral NGF, Wnt, RANKL, Dkk-1, ACTH, Leptin titer was measured and analyzed. After 2 weeks operation, the formation of callus was found at the fracture site, callus in TBI & Fr group was slightly higher than Fr group; however, there was no significant difference existed between the TBI & Fr and Fr groups. The ACTH level was significantly elevated in the TBI & Fr group than other groups and attained its peak at 1 week after operation, while the leptin was shown higher levels in Fr groups than TBI and TBI & Fr groups at 2 weeks after operation. The serum insulin level was markedly increased in all experimental groups during 1-3 days after surgery; at the meanwhile, the serum glucose level only significantly increased in the Fx and TBI groups at the 1 and 3 day after operation. The serum of NGF levels in the groups with TBI process (TBI and TBI & Fr groups) was significantly higher than those of the simple fracture group and control group. In the early stage of bone fracture, DKK-1 should be more active than Wnt-3a and NGF; later Wnt-3a and NGF became active to stimulate the osteoblasts for bone formation. After 3 day to 2 week of surgery, the RANKL process was drove to additional bone remodeling in accompany with bone formation. Conclusions: Through this project, the pathogenesis of increased rates of excessive bone healing in the patients with traumatic brain injury will be elucidated for the future study on clinical treatment in both traumatic brain injury and fracture healing. Keywords: Traumatic brain injury, fracture healing,
Author(s):
Yu-Ping Chen,Ching-Yun Chen,Cherng-Jyh Ke, Yuan-Hung Chao, Jui-Sheng Sun
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 161
Journal of Clinical & Experimental Orthopaedics received 161 citations as per google scholar report
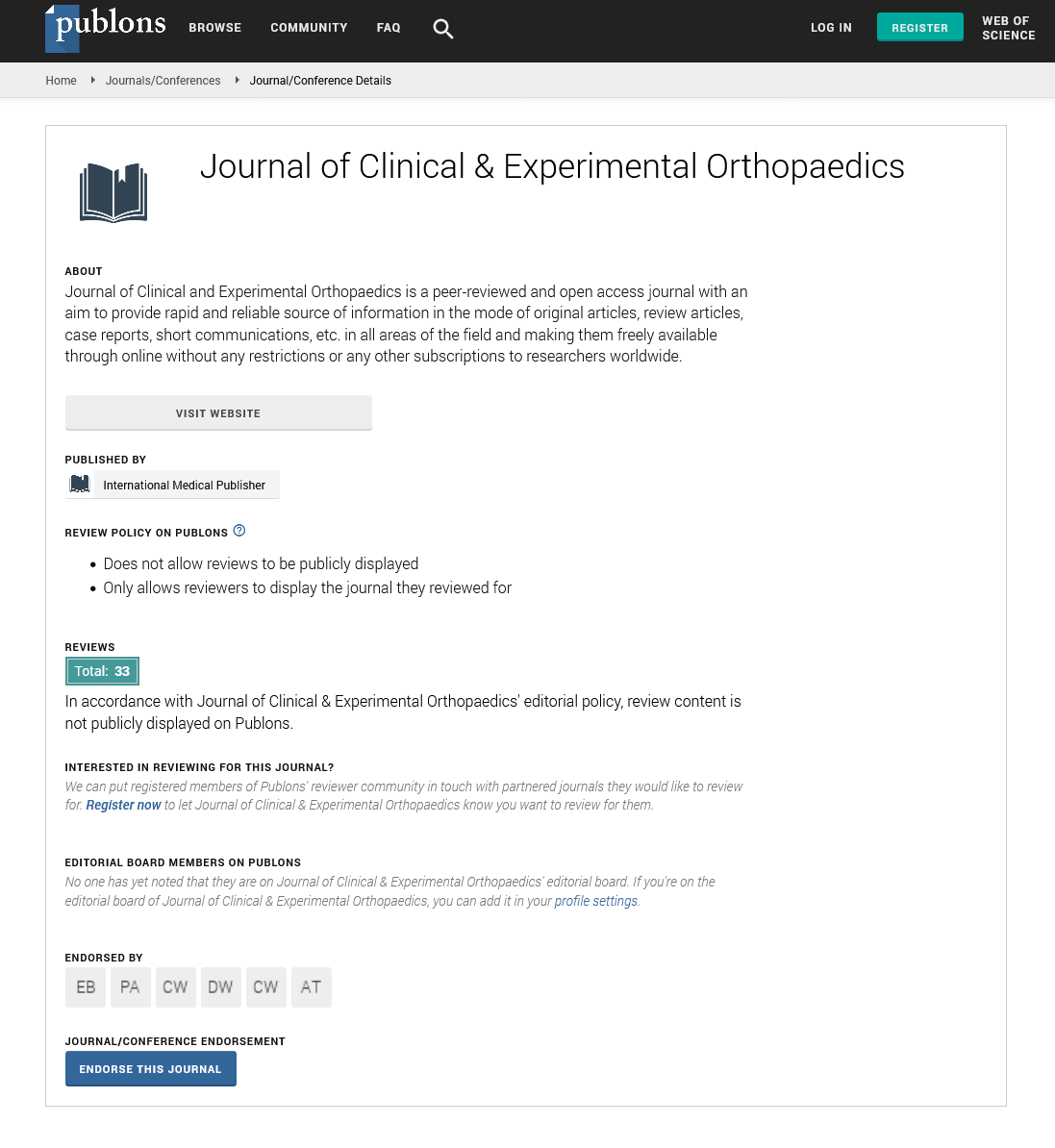
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences