Traumatic brain injury result in accelerated fracture healing: A Rat Model
Yu-Ping Chen,Ching-Yun Chen,Cherng-Jyh Ke, Yuan-Hung Chao, Jui-Sheng Sun
DOI10.4172/2471-8416.100006
Yu-Ping Chen1, Ching-Yun Chen2, Cherng-Jyh Ke3, Yuan-Hung Chao4, Jui-Sheng Sun5*
1Institute of Emergency and Critical Care Medicine, National YangMing University, Taipei, 11221 Taiwan (R.O.C.)
2Institute of Biomedical Engineering, College of Medicine and College of Engineering, National Taiwan University, Taipei, Taiwan (R.O.C)
3Center for Biomaterials and Entrepreneurship Development, China Medical University Hospital, Taichung, Taiwan, ROC.
4School and Graduate Institute of Physical Therapy, College of Medicine, National Taiwan University, Taipei, Taiwan.
5Department of Orthopedics, College of Medicine, National Taiwan University, Taipei, Taiwan (R.O.C.)
- *Corresponding Author:
- Jui-Sheng Sun MD, Ph.D
Department of Orthopedic Surgery
National Taiwan University Hospital. No.7
Chung-Shan South Rd., Taipei 10002
Taiwan, R.O.C
Tel: 886-2-23224112
E-mail: drjssun@gmail.com
Received date: November 04, 2015; Accepted date: December 17, 2015; Published date: December 21, 2015
Citation: Chen YP, Chen CY, Ke CJ, et al. Traumatic brain injury result in accelerated fracture healing: A Rat Model. J Clin Exp Orthop. 2015, 1:6. doi: 10.4172/2471-8416.100006
Copyright: © 2015 Chen YP, Chen CY, Ke CJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: In patients who have sustained a traumatic brain injury with an associated extremity fracture there is often a clinical perception that the rate of new bone formation around the fracture site is increased. In this study, we made a rat model of femoral fracture to investigate the serum factors changes in vivo. We examined the effects serum factors on fracture healing and the molecular signaling pathways that might link these two. Methods and Findings: Thirty-Six female Sprague-Dawley rats were randomly allocated into 4 groups; the non-operated control group, traumatic brain injury (TBI) group, bone fracture (Fr) group and the bone fracture/ TBI group (TBI & Fr) (n=9 per group). These animals were sacrificed at 6 weeks after experiments. Volume of callus in fracture was measured weekly with the Perkins volume formula at 2nd week after operation. The radiology imaging was interpreted by two or more senior orthopedic specialists. In vivo chemo taxis assay by serum samples collected at the 1, 3, 7 and 14 days, and 3rd, 4th, 6th week after surgery. Seral NGF, Wnt, RANKL, Dkk-1, ACTH, Leptin titer was measured and analyzed. After 2 weeks operation, the formation of callus was found at the fracture site, callus in TBI & Fr group was slightly higher than Fr group; however, there was no significant difference existed between the TBI & Fr and Fr groups. The ACTH level was significantly elevated in the TBI & Fr group than other groups and attained its peak at 1 week after operation, while the leptin was shown higher levels in Fr groups than TBI and TBI & Fr groups at 2 weeks after operation. The serum insulin level was markedly increased in all experimental groups during 1-3 days after surgery; at the meanwhile, the serum glucose level only significantly increased in the Fx and TBI groups at the 1 and 3 day after operation. The serum of NGF levels in the groups with TBI process (TBI and TBI & Fr groups) was significantly higher than those of the simple fracture group and control group. In the early stage of bone fracture, DKK-1 should be more active than Wnt-3a and NGF; later Wnt-3a and NGF became active to stimulate the osteoblasts for bone formation. After 3 day to 2 week of surgery, the RANKL process was drove to additional bone remodeling in accompany with bone formation. Conclusions: Through this project, the pathogenesis of increased rates of excessive bone healing in the patients with traumatic brain injury will be elucidated for the future study on clinical treatment in both traumatic brain injury and fracture healing. Keywords: Traumatic brain injury, fracture healing,
Keywords
Traumatic brain injury, fracture healing, rat model
Introduction
Fracture healing is a complex and orderly process. In orthopaedic practice, an accelerated rate of fracture healing has long been recognized to be associated with traumatic brain injury (TBI). Evidence for this association comes both from clinical practice and laboratory studies, where a relationship has been observed that the more rapid development of callus and the stimulation of bone forming cells after TBI [1,2]. Despite the alleged link between TBI and accelerated fracture healing is universally agreed, controversy still exists about the concerns with regard to both the validity of the findings and the process of the fracture healing [3]. As yet, the question of whether head injury genuinely results in accelerated fracture healing still remains unanswered [3-5].
When patients have both the TBI and bone fracture, there is often a clinical perception that osteogenic factors within cerebrospinal fluid (CSF) following TBI may be a possible source for systemic osteogenic factors [6]. The potential link between TBI and peripheral bone fracture is blood. The existence of humoral osteogenic factors following TBI has been suggested by the growth and osteogenesis promoting properties of blood from TBI subjects [6]. The candidates for the centrally released humoral factors remain the topic of speculation. Following TBI, many factors that may influence mesenchymal and osteoprogenitor proliferation are present in the serum in abnormal concentrations. These include some factors, such as nerve growth factor (NGF), Wnt, glucose, insulin, leptin, adrenocorticotropic hormone (ACTH), receptor-activator of NF-κB ligand (RANKL), Dickkopf-related protein 1 (DKK-1); these factors have a stimulatory effect in bone healing [7-10]. However, results are inconsistent and often reflect an incidental consequence of ossification or the blood-brain barrier (BBB) damage.
We think that it is worth making a patho-mechanism study; by which how the traumatic brain injury influences the expression of growth factors and consequently affect the speed of bone healing. Here, we made a rat model of femoral fracture to investigate the serum factors changes in vivo. In the studies described herein, we examined the effects serum factors on fracture healing and the molecular signaling pathways that might link these two. We postulated that pathway represents the convergence point between the two signaling cascades. Through this project, the pathogenesis of increased rates of excessive bone healing in the patients with traumatic brain injury will be elucidated for the future study on clinical treatment in both traumatic brain injury and fracture healing.
Materials and Methods
Study protocol
The experimental protocol was approved by the Institutional Animal Care and Use Committee of National YangMing University (Taipei, Taiwan). Thirty-Six female Sprague-Dawley rats (8 weeks old; 280 ± 20 gm) were purchased from the Laboratory Animal Center, National YangMing University (Taipei, Taiwan) and acclimated under standard laboratory conditions at 22 ± 2 °C and 50 ± 10% humidity. Standard rat chow and water were available ad libitum during the acclimation period. The animals were randomly allocated into 4 groups; the non-operated control group, traumatic brain injury (TBI) group, bone fracture (Fr) group and the bone fracture/ TBI group (TBI & Fr) (n=6 per group). These animals were sacrificed at 6 weeks after experiments.
Femoral Fracture Model
Femoral osteotomy and fixation were performed in the same manner as previously reports [11]. A transverse osteotomy was made at the mid-shaft of the left femur, and the fracture fragments were reduced and stabilized fixed using an intramedullary stainless steel wire (1.5 mm diameter, Synthes, Switzerland). The wire was cut on the surface of the intercondylar groove to avoid motion restriction of the knee joint. Rats were permitted unrestricted activity after recovery from anesthesia. The Sprague-Dawley rats were assuming its full weight; their activities were completely available after surgery.
Traumatic Brain Injury
The Sprague-Dawley rats were pre-anesthetized with zoletil (Virbac laboratories BP 27 - 06511 Carros, France) 30 mg/kg + xylazine (Rompun™, Bayer HealthCare LLC, Animal Health, Shawnee Mission, France) 10 mg/kg injunction under the anesthetized. The Sprague-Dawley skull was exposed and craniectomy was made laterally, at the point between the lambda and the Bregma, between the central suture and the left temporal ridge, using a 5 mm trephine. The exposed dura was subjected to a 5 mm-diameter. The scalp was closed with suture skin. After the traumatic brain injury surgery, the Sprague-Dawley rats were assumed completely available after surgery.
Radiology Measurement of callus volume
The Perkins volume formula was used as a measure of the volume of the fracture callus [5]. The Sprague-Dawley rats were anesthetized and took the radiology of anterior-posterior radiographs of all fractures. The volume of callus was calculated using the formula: 2πR1 (R2 - R1) L, (where R1 = femur radius, R2 = callus, L= length of callus). Volume of callus in fracture was measured weekly at 2nd week after operation. The radiology imaging was interpreted by two or more senior orthopedic specialists.
In vivo Chemotaxis Assay
In this assay, serum samples will be collected at the 1, 3, 7 and 14 days, and 3rd, 4th, 6th week after surgery. Peripheral blood 5 mL was collected from anesthetized Sprague-Dawley by means of rat tail and the serum was separated by centrifugation with 1500 rpm for 10 minutes at 4 ? to remove the cellular components. Finally, the serum was stored at -80°C until analysis. Serum Dickkopf 1 measured using a commercially available assay (Enzo Life Sciences, USA). NGF, Wnt, RANKL, ACTH, Leptin was measured by double antibody sandwich ABC-ELISA method (MILLIPLEX, Merck KGaA, Darmstadt, Germany). The OD values were proportional to the concentration of samples and read at 405 nm by using ELISA reader.
Statistical analysis
For all studies, P values were obtained using paired or unpaired two-tailed Student’s t-tests.
Results
Radiological analysis
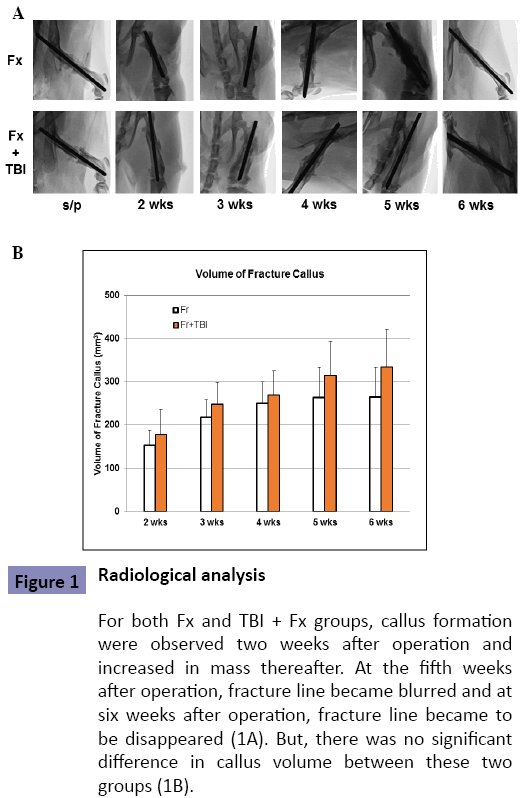
Callus dimensions were measured to determine if TBI affected fracture-healing. After 2 weeks operation, the formation of callus was found at the fracture site. As expected, callus in TBI & Fr group was slightly higher than Fr group. The callus gradually increased in both groups before 4 weeks. After 5 weeks operation, the fracture line became invisible, and the fracture calluses were partly absorbed and reduced comparing with those at 4 weeks (Figure 1A). Although there was a trend that the TBI & Fr group had a higher callus volume than Fr group; however, there was no significant difference existed between the TBI & Fr and Fr groups (Figure 1B; P>0.05).
Figure 1: Radiological analysis
For both Fx and TBI + Fx groups, callus formation were observed two weeks after operation and increased in mass thereafter. At the fifth weeks after operation, fracture line became blurred and at six weeks after operation, fracture line became to be disappeared (1A). But, there was no significant difference in callus volume between these two groups (1B).
Biochemical markers serum analysis
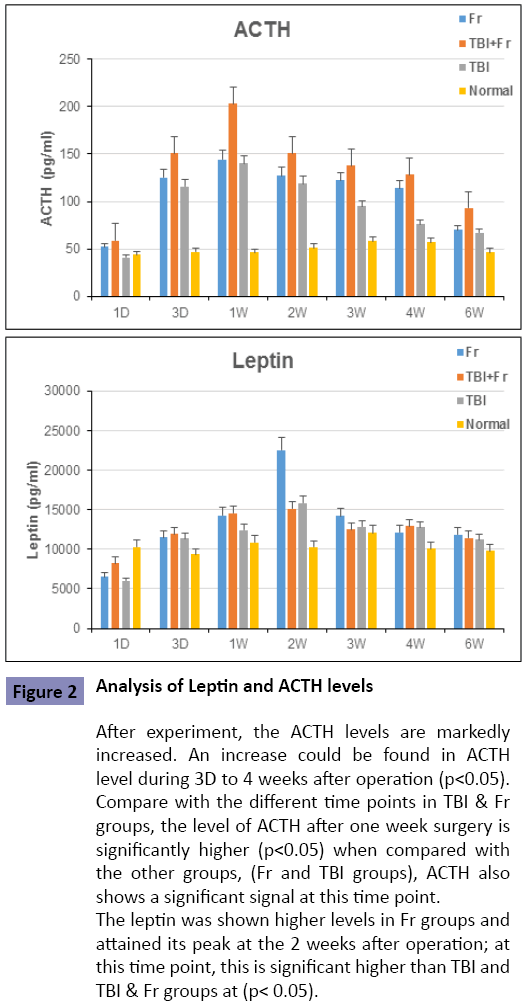
Analysis of Leptin and ACTH levels
Both the leptin and ACTH levels were markedly increased in all experimental groups after surgery. The ACTH level was significantly elevated in the TBI & Fr group than other groups and attained its peak at 1 week after operation, while the leptin was shown higher levels in Fr groups than TBI and TBI & Fr groups at 2 weeks after operation (P< 0.05; Figure 2). These results suggested that both central and peripheral tissues released factors might be involved in this study model.
Figure 2: Analysis of Leptin and ACTH levels
After experiment, the ACTH levels are markedly increased. An increase could be found in ACTH level during 3D to 4 weeks after operation (p<0.05). Compare with the different time points in TBI & Fr groups, the level of ACTH after one week surgery is significantly higher (p<0.05) when compared with the other groups, (Fr and TBI groups), ACTH also shows a significant signal at this time point.
The leptin was shown higher levels in Fr groups and attained its peak at the 2 weeks after operation; at this time point, this is significant higher than TBI and TBI & Fr groups at (p< 0.05).
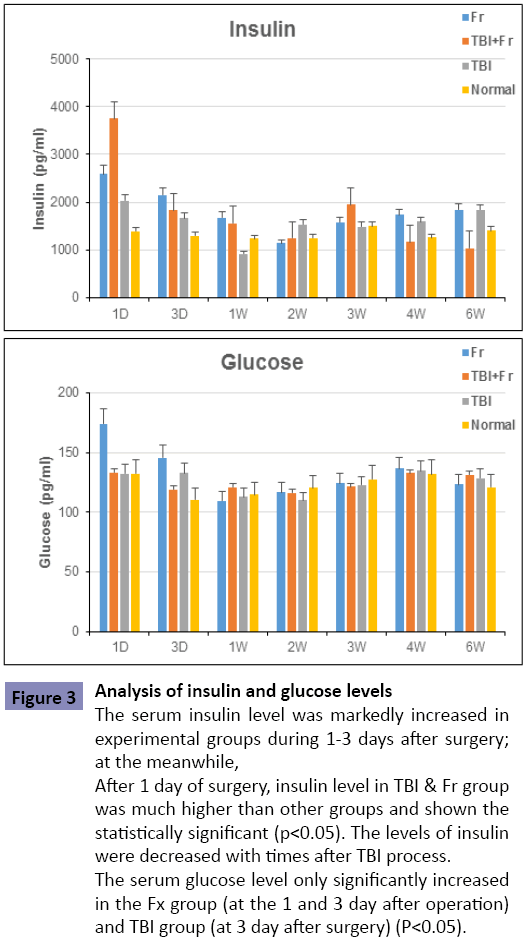
Analysis of insulin and glucose levels
The serum insulin level was markedly increased in all experimental groups during 1-3 days after surgery; at the meanwhile, the serum glucose level only significantly increased in the Fx and TBI groups at the 1 and 3 day after operation (P<0.05, Figure 3). Insulin and blood glucose have no direct relation to brain injury case but close to bone fracture. The body naturally tightly regulates blood glucose levels as a part of metabolic homeostasis [12].
Figure 3: Analysis of insulin and glucose levels
The serum insulin level was markedly increased in experimental groups during 1-3 days after surgery; at the meanwhile, After 1 day of surgery, insulin level in TBI and Fr group was much higher than other groups and shown the statistically significant (p<0.05). The levels of insulin were decreased with times after TBI process.
The serum glucose level only significantly increased in the Fx group (at the 1 and 3 day after operation) and TBI group (at 3 day after surgery) (P<0.05).
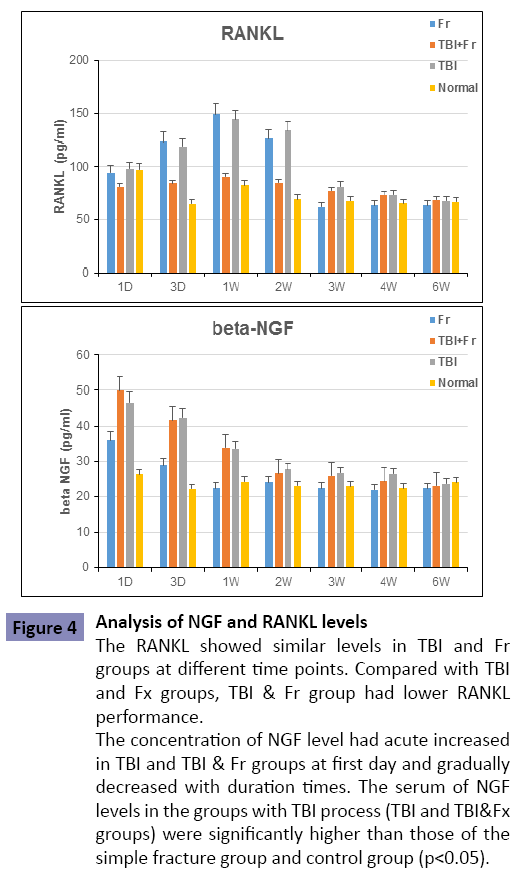
Analysis of NGF and RANKL levels
In this study, RANKL showed similar levels in TBI and Fr groups at different time points. Compared with TBI and Fr groups, TBI & Fr group had lower RANKL performance (Figure 4). It seems to approve that inactive RANKL in TBI & Fr group may promote the fracture healing.
Figure 4: Analysis of NGF and RANKL levels
The RANKL showed similar levels in TBI and Fr groups at different time points. Compared with TBI and Fx groups, TBI & Fr group had lower RANKL performance.
The concentration of NGF level had acute increased in TBI and TBI & Fr groups at first day and gradually decreased with duration times. The serum of NGF levels in the groups with TBI process (TBI and TBI&Fx groups) were significantly higher than those of the simple fracture group and control group (p<0.05).
The concentration of NGF level had acute increased in Fr, TBI and TBI & Fr groups at first day and gradually decreased with times. The serum of NGF levels in the groups with TBI process (TBI and TBI & Fr groups) were significantly higher than those of the simple fracture group and control group (P<0.05) (Figure 4). This result might suggest that NGF be synthesized or released in early stage of brain injury.
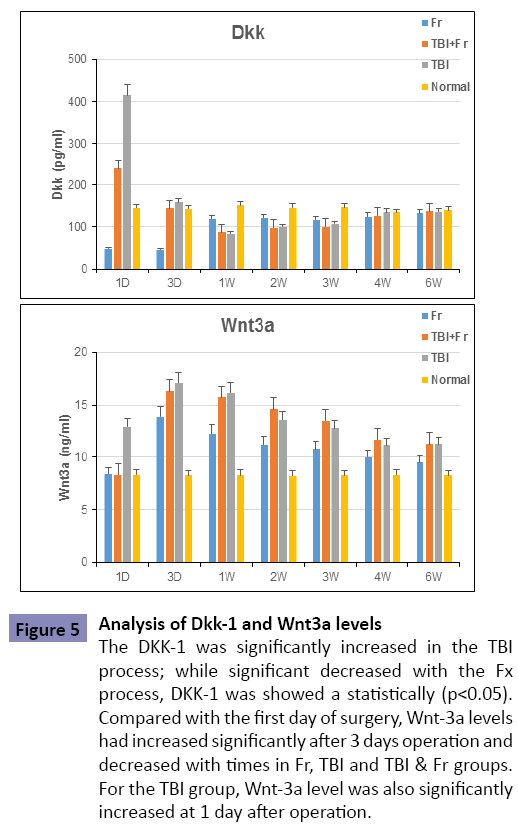
Analysis of Dkk-1 and Wnt-3a levels
Recent published data reveal that Wnt signaling pathway is activated during postnatal bone regenerative events, such as ectopic endochondral bone formation and fracture repair. DKK- 1 protein is an inhibition of the Wnt signaling pathway and association with osteolytic bone lesions. Furthermore, Wnt-3a can influence bone mass and bone development [13]. With TBI process, DKK-1 was shown to increase at statistically significant level (P<0.05); while with the Fr process, DKK-1 was significantly decreased (P<0.05). In our study, we also examined the effects of Wnt-3a that linked between TBI and fracture. Compared with the first day of surgery, Wnt-3a levels had increased significantly at 3 days after operation and decreased with times in Fr, TBI and TBI & Fr groups. For the TBI group, Wnt-3a level also significantly increased at 1 day after operation (Figure 5).
Figure 5: Analysis of Dkk-1 and Wnt3a levels
The DKK-1 was significantly increased in the TBI process; while significant decreased with the Fx process, DKK-1 was showed a statistically (p<0.05). Compared with the first day of surgery, Wnt-3a levels had increased significantly after 3 days operation and decreased with times in Fr, TBI and TBI & Fr groups. For the TBI group, Wnt-3a level was also significantly increased at 1 day after operation.
In the early stage of bone fracture, DKK-1 should be more activity than Wnt-3a and NGF; later Wnt-3a and NGF became active to stimulate the osteoblasts for bone formation. After 3 day to 2 week of surgery, the RANKL process was drove to additional bone remodeling in accompany with bone formation.
Discussion
The blood–brain barrier (BBB) is a highly selective permeability barrier that separates the circulating blood from the brain in the central nervous system (CNS). Generally, selective permeability of BBB can impede the passage of many molecules to prevent possible infection and the flow of CNS contents into the systemic circulation. However, when the BBB is damaged, molecules that are normally secluded within the CNS are released from the injured brain and can diffuse into the systemic circulation. If they have suitable biophysical parameters; it is possible that any insult to the CNS associated with BBB dysfunction represents a common mechanism for the release of osteogenic factors from the CNS and that severe trauma results in more widespread and significant injury, hence, higher rates of osteogenesis [9].
The studies published to date on this topic have been either retrospective, or analyses of case series with relatively small numbers of patients. Although three studies by different authors claim to have shown accelerated fracture healing after TBI [2,3,5]; the question that does traumatic brain injury result in accelerated fracture union is still a question not yet answered; there is a relative lack of sound information on the topic. It seems that the majority of authors propose that the new bone formed around fracture sites in patients with TBI could be a form of heterotopic ossification. Whether this heterotopic ossification goes on to form fracture callus and lead to bony union is a further debate and the rate at which this occurs causes most contention [9]. To date, although there was a consensus about the enhanced fracture healing seen in traumatic brain injury patients, the true mechanism behind this phenomenon remains unclear, and the precise factors are also still unknown.
Fracture healing is a complex process, involves cell, tissue proliferation and differentiation. A large number of genes in the above process are known, but many more remain to be discovered. However, previous studies on the effect in vitro of serum from patients with a traumatic brain injury have not reach an uniform conclusion [8]. Recently, an in vivo rat model of TBI and fracture established that the release of osteogenic humoral factors after TBI play a role in the early development of heterotopic ossification and fracture healing through the expansion of mesenchymal progenitors [6]. In our study, callus dimensions were measured to determine if TBI affected fracturehealing. Although there was a trend that the TBI & Fr group had a higher callus volume than Fr group; however, they did not reach a statistically significant difference (Figure 1).
Recent study reported that TBI induce BBB dysfunction, disruption of homeostasis, and changes of the levels of endogenous biochemical [14]. ACTH is a classic endocrine hormone; it secreted from the pituitary and stimulates cortisol in the adrenal gland. There is evidence that pituitary hormones, including ACTH, are key endocrine factors to regulate of bone turnover. Stress induced elevation in ACTH was observed and it represented the hyper-responsiveness to TBI stress (Figure 2). Specific in these TBI animal models, it is important to understand the neuroendocrine correlates that are likely to influence molecular markers following brain injury [15]. The hypothalamic leptin-dependent and peripheral mediators (through sympathetic nervous system) of leptin-dependent neuronal regulation inhibits bone formation [16]. Previous study have demonstrated significant leptin after rat brain injury is significantly higher than fracture group in the 2,4,8 weeks [11]. Leptin, a peptide hormone secreted by adipocytes, whereas high levels of leptin are accompanied by low levels of ACTH [15]. Previous studies have reported a relationship between leptin induced by brain injury and healing of bone tissue. They demonstrated elevated leptin expression within healing bone, particularly in the first 8 weeks of a rat model combining fracture and TBI [17]. But, our results did not present this phenomenon; in our study, the seral leptin levels were higher in all experimental groups; but most significantly increased in the Fr group at 2 weeks post-surgery (Figure 2).
Leptin regulates the four main hypothalamo-pituitary-peripheral axes - adrenal, thyroid, gonadal, and growth hormone axis - at different levels [18]. Previously, it was shown that the regulation of bone remodeling is mediated centrally by leptin [19], a peptide hormone secreted by adipocytes in response to insulin [20]. Although leptin acts through central and peripheral mechanisms to modulate glucose metabolism, leptin receptors are present in the β-cell, and their activation directly inhibits insulin secretion from these endocrine cells. The body naturally tightly regulates blood glucose levels as a part of metabolic homeostasis; the effects of leptin on insulin occur also in the long term, since this hormone inhibits insulin gene expression as well. Therefore, leptin can participate in glucose homeostasis owing to different levels of modulation of the pancreatic β-cell population [12].
The skeleton exerts an endocrine regulation of sugar homeostasis and energy metabolism that bone could influence glucose homeostasis by acting as an endocrine organ [21]. Osteocalcin (OCN) can promote proliferation of β cells, insulin secretion, and insulin sensitivity. Additionally OCN can also regulate the fat cells and male gonad endocrine activity and be regulated by insulin and the neural system. The skeleton has endocrine function via OCN and plays an important role in energy metabolism, especially in glucose metabolism [22]. Insulin signaling in osteoblasts has been shown recently to contribute to whole-body glucose homeostasis. Insulin resistance in osteoblasts led to a decrease in circulating levels of the active form of osteocalcin, thereby decreasing insulin sensitivity in skeletal muscle [23]. Insulin signaling in osteoblasts enhances osteocalcin activity and impacts glucose homeostasis by promoting the ability of osteoblasts to enhance bone resorption [22]. Insulin signaling in osteoblasts enhances osteocalcin activity and impacts glucose homeostasis by promoting the ability of osteoblasts to enhance bone resorption [22]. In this study, the serum insulin and glucose level also significantly affected by experimental procedures (Figure 3).
Receptor activator of nuclear factor-κB ligand (RANKL) is secreted by osteoblasts. In normal bone remodeling, osteoblasts produce RANKL, which binds to the RANK receptor on osteoclast to activate osteoclast precursors [24]. Associated RANKL/RANK system in the brain is also expressed in the central nervous system (CNS). The RANKL/RANK indeed controls fever, in the central nervous system (CNS) [25]. But the functional was unknown. In this study, RANKL showed similar levels in TBI and Fr groups at different time points. Compared with TBI and Fr groups, TBI & Fr group had lower RANKL performance (Figure 4). It seems to approve that inactive RANKL in TBI & Fr group promote the fracture healing.
In clinic, many scholars positively seek the bridge factor of the central nervous system and bone metabolism. Studies have shown that the damaged brain tissue or the pituitary gland secretes a large number of growth factors and inflammatory cells; they can release and secrete a variety of cytokines which promote the healing of fractures by fluid circulation and paracrine in the fracture ends [8,26]. And then, the serum of patients with limb fracture combined with brain injury cans significantly promoting the mitosis of osteoblast cells and proliferation of the bone marrow stem cell [27]. The serum of NGF, EGF levels significantly increased when limb fracture combined with brain injury, so EGF and NGF may be involved in the process of fracture healing [7]. In our study, the concentration of NGF levels in the groups with TBI process (TBI and TBI & Fr groups) were significantly higher than those of the simple fracture group and control group (P<0.05) (Figure 4). This result might suggest that NGF be synthesized or released in early stage of brain injury.
During the past decade, secreted signaling molecules of the Wnt family have been widely investigated and found to play a central role in controlling embryonic development processes. Wnt signaling pathway also plays a pivotal role in the regulation of bone mass. Dysregulation of this pathway greatly inhibits bone formation and healing process. Interestingly, activation of Wnt pathway has potential to improve bone healing, but only utilized after mesenchymal cells have become committed to the osteoblast lineage [13]. Wnt antagonist Dickkopf-1 (Dkk1) is an important role on skeletal development and bone remodeling. It inhibits the WNT signaling pathway in the differentiation of osteoblasts [28]. The Dkk1 and -2 facilitate osteoclastogenesis by enhancing RANKL/RANK and M-CSF/c-Fms interactions [29]. Our results showed that DKK-1 should be more activity than Wnt-3a and NGF In the early stage of bone fracture; later Wnt-3a and NGF became active to stimulate the osteoblasts for bone formation. After initial increase during the 3 day to 2 week after surgery, the RANKL process was driven to additional bone remodeling in accompany with bone formation (Figure 5).
Conclusion
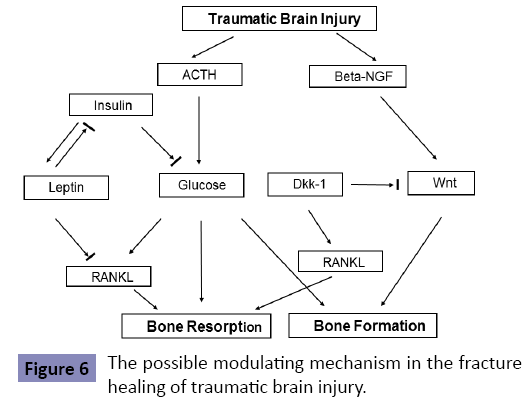
We concluded that when patients suffer from traumatic brain injury and fracture, there has a tends to have faster fracture healing. We also demonstrated that when fractured cases suffered accompanied with traumatic brain injury, the in vivo regulation of ACTH, insulin, leptin, NGF, Wnt/DKK-1 and RANKL is complex and sensitive [30]. The stress activates immune/inflammatory response and stimulates pituitary cortisol including ACTH. Its effects are increased release of corticosteroids. Corticosteroids secretion glucose. Leptin lets osteoblasts inhibits osteoclast generation by modulating the pro-osteoclastogenesis RANK by marrow osteoblastic cells [31]. In conclusion, we suggest that ACTH, insulin, leptin, NGF, Wnt/DKK-1 and RANKL can all actively regulate the fracture repair in traumatic brain injury. Perhaps the rats that suffer double stress tend to induce a release of complex and sensitive stress hormone response (Figure 6). But, further in vitro and in vivo studies are still needed to clarify the modulating mechanism in the process of fracture healing.
Competing Interests
There is no conflict of interest that could inappropriately influence the work reported in this manuscript.
Author Contributions Statement
Dr. Sun, JS is in charge of research design, interpretation of data, drafting the paper or critical revision, and approval of the submitted and final versions. Miss Chen, YP is the main person for the initiation of research design, the acquisition and primary analysis or interpretation of data and also drafting the paper. Dr. Chen, CY, Dr. Ke, CJ and Dr. Chao YH support us all the research design, interpretation of data, and also actively join all research design and data mining works. All authors also have read and approved the final submitted manuscript.
Acknowledgements
The authors thank the Second Core Lab. of National Taiwan University Hospital for their kindly technical support during this study. This study was financially supported by Scientific Research from Ministry of Science and Technology, Taiwan, ROC and National Yang-Ming University, Taiwan, ROC.
References
- Bidner SM, Rubins IM, Desjardins JV, Zukor DJ, Goltzman D (1990) Evidence for a humoral mechanism for enhanced osteogenesis after head injury. J Bone Joint Surg Am 72: 1144-1149.
- Newman RJ, Stone MH, Mukherjee SK (1987) Accelerated fracture union in association with severe head injury. Injury 18: 241-246.
- Spencer RF (1987) The effect of head injury on fracture healing. A quantitative assessment. J Bone Joint Surg Br 69: 525-528.
- Smith R (1987) Head injury, fracture healing and callus. J Bone Joint Surg Br 69: 518-520.
- Perkins R, Skirving AP (1987) Callus formation and the rate of healing of femoral fractures in patients with head injuries. J Bone Joint Surg Br 69: 521-524.
- Toffoli AM, Gautschi OP, Frey SP, Filgueira L, Zellweger R (2008) From brain to bone: evidence for the release of osteogenichumoral factors after traumatic brain injury. Brain Inj 22: 511-518.
- Zhuang YF, Li J (2013) Serum EGF and NGF levels of patients with brain injury and limb fracture. Asian Pac J Trop Med 6: 383-386.
- Boes M, Kain M, Kakar S, Nicholls F, Cullinane D, et al. (2006) Osteogenic effects of traumatic brain injury on experimental fracture-healing. J Bone Joint Surg Am 88: 738-743.
- Morley J, Marsh S, Drakoulakis E, Pape HC, Giannoudis PV (2005) Does traumatic brain injury result in accelerated fracture healing? Injury 36: 363-368.
- Daoud H, Alharfi I, Alhelali I, Charyk Stewart T, Qasem H, et al. (2014) Brain injury biomarkers as outcome predictors in pediatric severe traumatic brain injury. Neurocrit Care 20: 427-435.
- Wang L, Yuan JS, Zhang HX, Ding H, Tang XG, et al. (2011) Effect of leptin on bone metabolism in rat model of traumatic brain injury and femoral fracture. Chin J Traumatol 14: 7-13.
- Marroquí L, Gonzalez A, Ñeco P, Caballero-Garrido E, Vieira E, et al. (2012) Role of leptin in the pancreatic β-cell: effects and signaling pathways. J MolEndocrinol 49: R9-17.
- Chen Y, Alman BA (2009) Wnt pathway, an essential role in bone regeneration. J Cell Biochem 106: 353-362.
- Yang S, Ma Y, Liu Y, Que H, Zhu C, et al. (2012) Arachidonic acid: a bridge between traumatic brain injury and fracture healing. J Neurotrauma 29: 2696-2705.
- Griesbach GS, Hovda DA, Tio DL, Taylor AN (2011) Heightening of the stress response during the first weeks after a mild traumatic brain injury. Neuroscience 178: 147-158.
- Takeda S, Elefteriou F, Levasseur R, Liu X, Zhao L, et al. (2002) Leptin regulates bone formation via the sympathetic nervous system. Cell 111: 305-317.
- Wei Y, Wang L, Clark JC, Dass CR, Choong PF (2008) Elevated leptin expression in a rat model of fracture and traumatic brain injury. J Pharm Pharmacol 60: 1667-1672.
- Khan SM, Hamnvik OP, Brinkoetter M, Mantzoros CS (2012) Leptin as a modulator of neuroendocrine function in humans. Yonsei Med J 53: 671-679.
- Elefteriou F, Ahn JD, Takeda S, Starbuck M, Yang X, et al. (2005) Leptin regulation of bone resorption by the sympathetic nervous system and CART. Nature 434: 514-520.
- Cammisotto PG, Bukowiecki LJ (2002) Mechanisms of leptin secretion from white adipocytes. Am J Physiol Cell Physiol 283: C244-250.
- Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, et al. (2007) Endocrine regulation of energy metabolism by the skeleton. Cell 130: 456-469.
- Shao J, Wang Z, Yang T, Ying H, Zhang Y, et al. (2015) Bone Regulates Glucose Metabolism as an Endocrine Organ through Osteocalcin. Int J Endocrinol 2015: 967673.
- Wei J, Ferron M, Clarke CJ, Hannun YA, Jiang H, Blaner WS, et al. Bone-specific insulin resistance disrupts whole-body glucose homeostasis via decreased osteocalcin activation. J Clin Invest. 2014; 124(4): 1-13.
- Singh PP, van der Kraan AG, Xu J, Gillespie MT, Quinn JM. (2012) Membrane-bound receptor activator of NF?B ligand (RANKL) activity displayed by osteoblasts is differentially regulated by osteolytic factors. BiochemBiophys Res Commun. 422(1): 48-53.
- Hanada R, Hanada T, Sigl V, Schramek D, Penninger JM (2011) RANKL/RANK-beyond bones. J Mol Med (Berl) 89: 647-656.
- Onodera S, Nishihira J, Yamazaki M, Ishibashi T, Minami A. (2004) Increased expression of macrophage migration inhibitory factor during fracture healing in rats. Histochem Cell Biol.121(3): 209-217.
- Gautschi OP, Cadosch D, Frey SP, Skirving AP, Filgueira L, et al. (2009) Serum-mediated osteogenic effect in traumatic brain-injured patients. ANZ J Surg 79: 449-455.
- Monroe DG, McGee-Lawrence ME, Oursler MJ, Westendorf JJ (2012) Update on Wnt signaling in bone cell biology and bone disease. Gene 492: 1-18.
- Fujita K, Janz S (2007) Attenuation of WNT signaling by DKK-1 and -2 regulates BMP2-induced osteoblast differentiation and expression of OPG, RANKL and M-CSF. Mol Cancer 6: 71.
- Ek O, Muhr M, Hulting AL, Jansson KÅ (2013) Traumatic brain injury and fracture. Lancet 381: 874.
- Andermahr J, Elsner A, Brings AE, Hensler T, Gerbershagen H, et al. (2006) Reduced collagen degradation in polytraumas with traumatic brain injury causes enhanced osteogenesis. J Neurotrauma 23: 708-720.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences